
The benefits of mammography are well documented and widely understood. Following a screening mammogram, the patient may be called back for additional imaging to further investigate the findings. Some women, however, decide to forego recommended follow-up breast imaging for any number of reasons.
For example, she may not understand the need for the follow-up exam, be afraid of the results, have difficulty finding the time or scheduling the exam, or is reluctant or unable to incur the additional cost.
Although preventative exams such as screening mammograms are covered by most insurance plans, the cost of a diagnostic follow-up exam is often an out of pocket expense, particularly with high-deductible health plans (HDHPs).
Out of pocket costs deter women from seeking recommended care
According to a recent study, 21% of women said they would skip indicated follow-up imaging if they knew they had to pay a deductible. These results reflect how some breast imaging practices have noticed a decline in patient adherence to recommended diagnostic imaging following abnormal screening since the adoption of the Affordable Care Act. Furthermore, 18% said they would skip screening mammography altogether if they knew they had to pay a deductible for follow-up imaging or biopsy tests.
 Whether these troubling survey results are a precursor to an uptick in delayed breast cancer detection remains to be seen. Regardless, as HDHPs have grown in popularity, this study "demonstrates that out-of-pocket payments will discourage people, especially those belonging in the most vulnerable populations, from completing the last steps in the breast cancer screening process," Michael Ngo, MD, the study's lead author and radiology resident at Boston Medical Center and Boston University Chobanian & Avedisian School of Medicine said.
Whether these troubling survey results are a precursor to an uptick in delayed breast cancer detection remains to be seen. Regardless, as HDHPs have grown in popularity, this study "demonstrates that out-of-pocket payments will discourage people, especially those belonging in the most vulnerable populations, from completing the last steps in the breast cancer screening process," Michael Ngo, MD, the study's lead author and radiology resident at Boston Medical Center and Boston University Chobanian & Avedisian School of Medicine said.
Decision to delay can lead to later stage diagnosis
Similarly, when additional screenings or follow-up tests are recommended because of breast density, family history, or other reasons, a majority of women are forced to pay out of pocket.
As a result, many who cannot afford this cost will choose to delay or forego these additional tests, and that decision to delay screening can lead to later stage diagnosis. Appropriate and timely follow-up after a positive screening mammogram is crucial: breast cancer screening via mammography is only effective in reducing mortality if followed by timely diagnosis and treatment.
Delayed follow-up after a positive screening mammogram may contribute to disparities in breast cancer outcomes and subsequent mortality since follow-up times of 3-6 months has been associated with larger tumor size at diagnosis and reduced survival.
Help is on the way
Fortunately, legislation is being put forth that requires these important follow-up tests to be covered by insurance, potentially reducing existing health inequities and improving access for women with dense breasts or other heightened risk factors for breast cancer.
In December 2022, Congresswoman Rosa DeLauro (CT), Congressman Brian Fitzpatrick (PA), and journalist Katie Couric introduced legislation that would ensure all health insurance plans cover screening and diagnostic mammograms and breast ultrasounds and MRIs with no cost-sharing. Called the Find It Early Act, this legislation is aimed at improving early breast cancer detection for all women.

What can be done to help put women’s minds at ease, making the need for follow-up exams more precise and reducing avoidable callbacks?
For the patient, returning for follow-up imaging is a stressful event. In a 2021 survey of women across the US who were called back following a screening mammogram, 33% said the callback made them feel scared, frightened, terrified, afraid or fearful.
Taking the guesswork out of interpreting mammograms can ease the stress that patients as well as technologists and radiologists experience. It not only saves time but also decreases the chance of misinterpretation and avoidable callbacks.
As Christina Jacobs, MD, Director of Breast Imaging of Bronson Health System, states "Reducing avoidable callbacks means we can minimize inconvenience, anxiety, and additional radiation exposure."
Skin markers help reduce questions that lead to additional screening
"The use of skin markers during mammography is a simple and effective way to identify palpable masses, moles, prior surgical scars, nipples, and other areas of concern or pain. Their consistent use improves communication across the care team and can help make interpreting mammograms more efficient and accurate," explains Joseph C. Benjamin, MD, Specialist in Breast Imaging and Lead Interpreting Physician at Mercy Health, Cincinnati, Ohio.
Underscoring the importance of skin markers for mammography, a 2021 survey of women across the US showed 79% of respondents who had a skin marker placed during their mammogram felt it was "Absolutely Essential" or "Very Important" that their imaging center use skin markers.
Implementing a marking system that consists of unique and distinctive shapes provides certainty when interpreting images
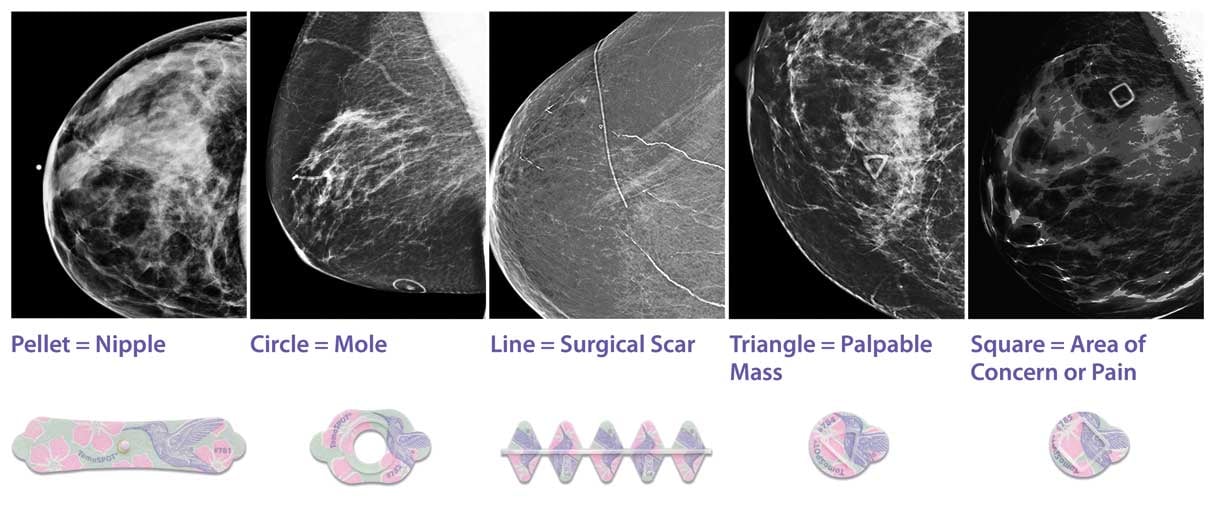
The Beekley Skin Marking System® has five different shapes that uniquely identify the area of interest on the breast: a circle for a raised area on the skin such as a mole, a line for a previous surgery, a triangle for a palpable mass, a solid pellet for the nipple, and a square for non-palpable areas of concern or pain. These markers, each with a unique shape for a specific purpose, help save time, improve communication, and positively impact clinical efficacy.
If you would like to learn more about the Beekley Skin Marking System for Mammography, contact your Beekley Medical Account Manager at 1.800.233.5539 or email info@beekley.com.

Maria Shonyo
President, Vela Technologies, LLC
