As someone whose father has gone through conventional external beam radiotherapy (EBRT), I can tell you that the physical and emotional toll it takes on patients and their caregivers is no easy journey.
Going to appointments multiple times a week, for hours at a time was daunting for my father, and some days the side effects were so bad he would swear he was not going back.
Years later, the outcome was worth the “hassle” as he has been in remission since. However, after discovering Targit-IORT (targeted intraoperative radiotherapy treatment) for breast cancer, I wish there was something similar for every type of cancer.
Radiation treatment in a single dose
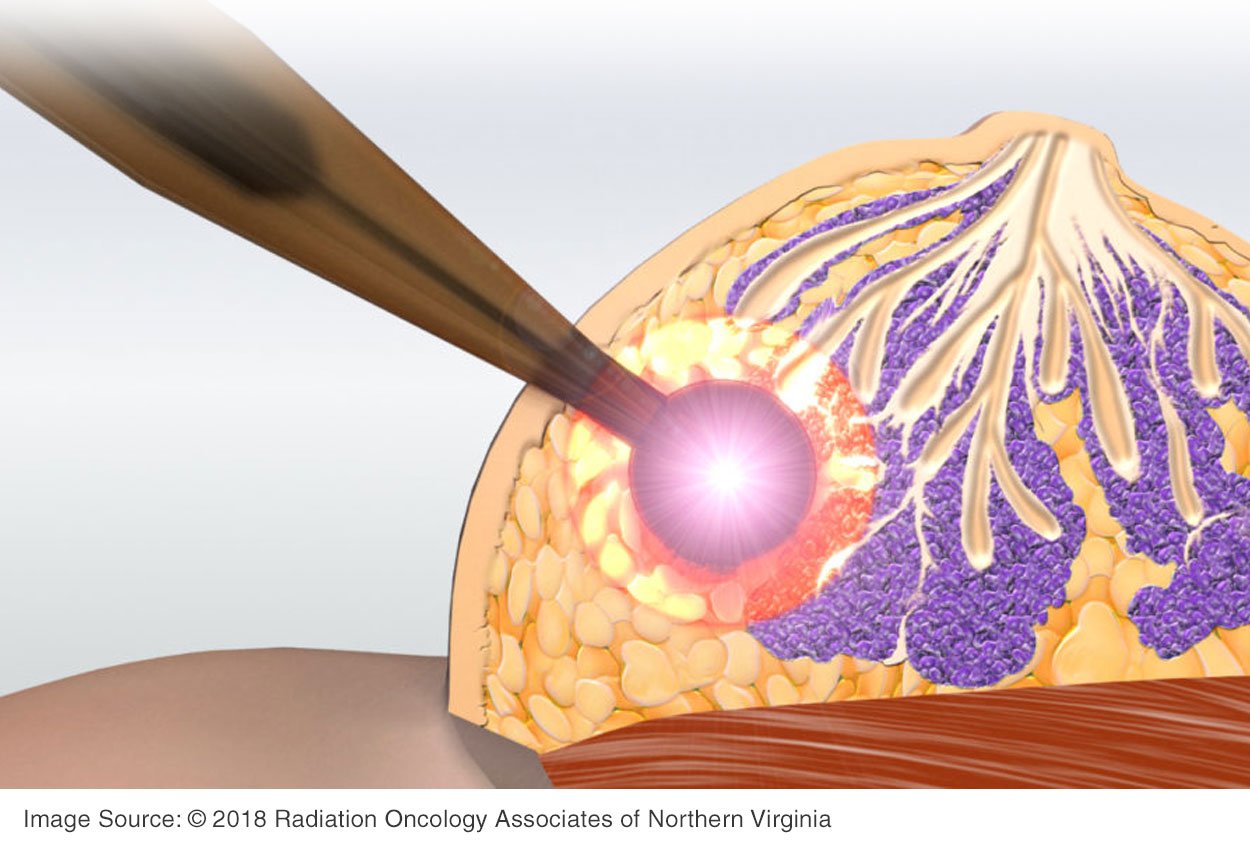
Under the same anesthetic as a lumpectomy, a ball-shaped device is placed inside the breast after the tumor is removed, directly where the cancer had been. The single-dose treatment lasts an additional 20-30 minutes.
Delivering the radiation immediately to the site where the tumor was can reduce the adverse effects of surgical trauma, resulting in quicker recovery time. It also reduces the amount of radiation a patient is exposed to and makes the site less conducive for cancer growth.
Targeted therapy, less side effects, speedier recovery than traditional radiation treatment
 Targit-IORT or IORT for short, delivers a high dose of radiation at the same time as the patient’s lumpectomy eliminating multiple sessions of traditional radiation treatment as well as limiting the exposure to radiation on surrounding healthy tissue.
Targit-IORT or IORT for short, delivers a high dose of radiation at the same time as the patient’s lumpectomy eliminating multiple sessions of traditional radiation treatment as well as limiting the exposure to radiation on surrounding healthy tissue.
IORT is believed to have fewer side effects overall compared to EBRT, with no difference in survival or likelihood of the cancer returning.
Avoiding the mild to moderate fatigue, skin irritation, and breast swelling that may accompany EBRT is a big reason breast cancer patients may opt for IORT instead. In fact, one patient recalled her chronic migraines being worse than the side effects from IORT.
According to paper published in the British Journal of Cancer, 8 out of 10 patients who receive IORT will not need any additional post-operative EBRT and they avoid scattered radiation that can occur during EBRT which can damage nearby healthy vital organs.
This essentially gives breast cancer patients their lives back quicker. IORT reduces the amount of time a patient spends in the hospital after a normal lumpectomy and it enables them to recover faster, meaning they can get back to their regular life in a shorter amount of time.
In one patient story, a 60-year-old self-employed psychotherapist patient from London wrote how grateful she was to be able to return to work a within two weeks of her operation and IORT treatment and that she experienced very minimal side effects. Other patient stories echo that theme, especially how much they appreciated not having to travel to the hospital daily for weeks of radiotherapy.
IORT also played a role during the height of the COVID-19 pandemic. It helped dramatically reduce the amount of times patients were in the hospital, decreasing the chances of contracting and/or spreading the virus.
Interestingly, both IORT and EBRT lower the likelihood of death if the patient were to develop cardio-vascular disease after a lumpectomy. It is thought to be because both types of therapy change the microenvironment in the lumpectomy wound.
Narrow eligibility criteria means IORT is not for everyone - age, tumor size matters
As with most procedures, there are certain criteria patients must meet before their doctor decides which post-surgical cancer treatment is best for them.
In the case of IORT, the general criteria are that a patient must be at least 45 years old, have a tumor smaller than 2.5cm, and have no evidence of cancer in the lymph nodes.
"With TARGIT-IORT, the majority of patients presenting with early localized breast cancer will never need any further radiotherapy," according to Professor Jeffrey S. Tobias, professor of clinical oncology, UCL and UCLH.
Despite the narrow criteria, adoption of IORT is growing... To date roughly 45,000 patients across 38 countries have undergone this procedure.
While radiation therapy remains the standard of care for treating breast cancer, it is our hope that early detection through annual screening mammograms enables more breast cancer patients to have the option of IORT so that they can lead fuller, better lives as breast cancer survivors that much sooner.
Related articles:

Megan Sargalski
Marketing Communications Specialist
