
Around the country, new medical buildings seem to break ground and open for business in record breaking time. With new locations being built all around us, healthcare systems are expanding satellite offices outside the hospitals, providing additional services as well as more flexible scheduling of appointments.
These increased options for care and convenience offer a one-stop-shopping approach to personalized healthcare with the ultimate goal of providing greater patient service.
However, an increasing challenge that occurs with expansion, is the ability to establish standardized protocols across the entire healthcare system.
This is particularly true in mammography where communication methods can vary between groups of technologists and radiologists who rotate between various locations.
“What site am I reading at today, and what protocols do they follow?”
One breast radiologist shared the phrase that often enters her mind at the start of her day: “What site am I reading at today, and what protocols do they follow?” This ever-evolving practice of bouncing between locations intensifies the need for uniformity.
Dr. Amanda Squires, a radiologist with Vista Radiology shared her perspective on why consistency matters in mammography today.
“I get a lot of the other centers’ patients when they’re in need of treatment and it takes me additional time to figure the case out, especially when there is a lack of standardization.
“For example, what does that BB mean? Is it a nipple, palpable, skin lesion, etc.? In addition to all the other things I am concerned with identifying, I'm also having to figure out how big is the lesion? When were the priors? These are a few among the many questions that constantly arise.
“There are always various pieces to be put together to be sure that I am contributing to the case appropriately -doing a wire localization, ordering an MRI to define extent, etc.”
"Our energy should be focused on the things that are hard, not wasted on the parts that are easy"
According to Dr. Squires, ambiguity with interpretation as to which markers are used for what can detract from the real focus which should be on the patient and the more important questions she should be concentrating on.
In her opinion, “anything that can be automated, should be. This allows more time to address the important questions that require us to reason our way through. In our mission to find cancers at their earliest stage, our energy should be focused on the things that are hard, not wasted on the parts that are easy.
“Implementing a consistent communications protocol with skin markers across all sites would save me from having to reference that question in the report. Enhanced consistency which results in saving me time is so important and very much appreciated. I think this is one of the main reasons that the BI-RADS standards were created.”
Standardization of communication matters
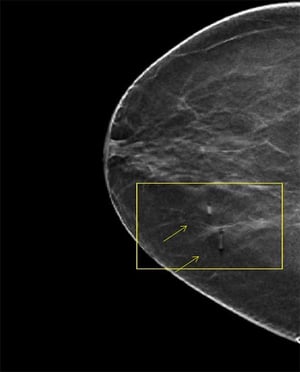 |
| 1.5 metallic pellet marker indicating moles on a digital breast tomosynthesis (DBT) image slice |
The purpose behind BI-RADS was to standardize the imaging reporting language and reduce confusion in image interpretation by providing a common language among radiologists and imaging practices - enabling reliable communication to referring clinicians regarding the significance of findings and management recommendations.
Much like the language of BI-RADS, the ACR continues to update their Appropriateness Criteria and Practice Parameters to provide guidance for uniform practices in breast imaging.
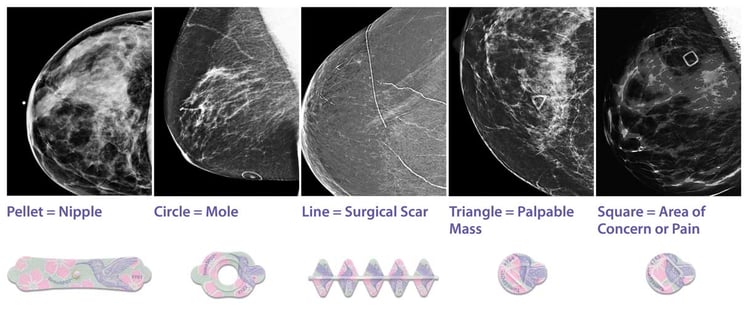
It was for this reason the Beekley Skin Marking System for Mammography® was developed; to assist radiologists in their image interpretation by communicating areas of interest at a glance.
Five distinct, recognizable shapes clearly define and streamline the communication process between technologist and radiologist: a circle for moles, a line for surgical scars, a pellet for nipples, a triangle for palpable masses, and a square for non-palpable areas of concern.
A visible language that goes beyond the intake sheets
While charting is an important part of documenting patient history, the added value and benefit of a consistent skin marking protocol that can be seen directly on the patient’s images from year to year is increasingly more valuable.
While many patients may stay at the same facility for follow up diagnostic visits or routine screening year after year, it is common to get second opinions or even see different doctors within the same practice.
When patients request their images from prior examinations from other facilities, there isn’t always a guarantee that what radiologists see is enough to answer all their questions. Full reports do not always accompany those images, and one person may use a “BB” to mark a palpable mass as opposed to a radiolucent triangle.
If facilities within the same system do not have the same communication protocols, image interpretation can be negatively impacted – running the risk of unnecessary additional image for clarification, false positives, or false negatives.
Learn more about standardization with skin markers and why they continue to add value in image interpretation in the era of 3D Breast Tomosynthesis with Advanced Skin Marking in Breast Tomosynthesis and MRI, a self-guided CE activity approved by the ASRT for 1 Category A continuing education credit, compliments of Beekley Medical.
Related articles:

Kathy Kaschuluk
Product Manager
