
There’s an adage in healthcare “If it’s not documented, it didn’t happen.” Documentation that is a complete, accurate, timely account of a patient’s condition or status not only provides efficient and accurate communication to all on that patient’s medical team, it is also the number one defense against potential litigation.
In his JACR article, “Hiding in the Hedges: Tips to Minimize Your Malpractice Risks as a Radiologist,” author Jonathan Mezrich, MD, JD, Assistant Professor in the Emergency Radiology section of the Department of Radiology and Biomedical Imaging at Yale University School of Medicine and former practicing lawyer emphasizes “clarity” and “communication” among the 5 Cs radiologists should try to adhere to on a daily basis. A recent study noted that roughly 70% of all radiologists experience at least 1 malpractice lawsuit in their career.
When it comes to screening for breast cancer, communication and documentation can mean the difference between a missed diagnosis or a misdiagnosis.
The special challenge for specialists in breast imaging
Half-jokingly referred to as trying to find a snowflake in a snow storm, mammography remains one of the more difficult imaging modalities to practice, despite advances in technology that allow greater visualization of breast tissue detail than ever before.
We had the opportunity to hold a round table discussion about the importance of communication in mammography with several dedicated breast radiologists at the 24th Annual Mammography in Santa Fe conference held August 5-9, 2019.
The importance of standardization and documentation in mammography
Two of the major themes emerging from this discussion were the importance of standardization and documentation.
 One of the panelists* described how she used to get sticky notes relating to technologists’ assessment of the patient - for example explaining how motion artifact due to the patient having Parkinson's and couldn't hold still. While the panelist appreciated the information, she pointed out that "those sticky notes are going to be long gone if, and when, I ever need to remember why I didn't repeat those films that normally would have been repeated. If I'm sitting in court in 5 years, those sticky notes are not going to help me."
One of the panelists* described how she used to get sticky notes relating to technologists’ assessment of the patient - for example explaining how motion artifact due to the patient having Parkinson's and couldn't hold still. While the panelist appreciated the information, she pointed out that "those sticky notes are going to be long gone if, and when, I ever need to remember why I didn't repeat those films that normally would have been repeated. If I'm sitting in court in 5 years, those sticky notes are not going to help me."
One way to permanently document communication between technologist and radiologist is through the use of mammography skin markers to augment the patient intake sheet regarding the location of visual findings, palpable findings, and previous surgical sites.
Architectural distortion in DBT; how scar markers help radiologists identify old surgeries
When we asked the panelists what they thought about the ACR amending their practice parameters regarding skin markers to recommend that “facilities should require consistent use of radiographically distinct markers to indicate palpable areas of concern, skin lesions, and surgical scars,’’ we learned that the majority of the panelists embraced the addition of consistent marking of post-surgical scars to the recommendations based on their experience with transitioning to Digital Breast Tomosynthesis (DBT).
Post-surgical scarring in the parenchyma becomes less visible on the mammographic image over time, especially with benign biopsies. It wasn’t uncommon for imaging facilities to stop marking the surface scar as a point of reference a few years after the surgery.
However, as another of the panelists* explained, “once transitioning to 3D, marking scars becomes critical because with DBT, the scars become so much more pronounced. There are a lot of times you don’t sees scars in 2D, but with Tomo, you see them- I’ve seen plenty of massive spiculations from scar tissue, even from benign things that were removed.”
“I think marking any scar, whether it was a benign or malignant process is really crucial. The extra work involved in additional imaging for clarification of a previous surgical site, not to mention the anxiety on the part of the patient, could have been avoided if somebody had marked the scar. It’s much more efficient and cost-effective to mark it beforehand, rather than call the patient back.”
Consistent use of scar markers helps with year-to-year image comparison
When it comes to comparing year-to-year images, Jean Weigert, MD (Jefferson Radiology, an affiliate of MEDNAX®, Hartford, CT) emphasized “Rather than only mark for a year or two after surgery, it is important for me to have consistency and helps with my comparison from year to year when I see a scar marker.”
Amanda Squires, MD (Vista Radiology, Knoxville, TN) agreed that the consistent use of scar marking is “incredibly helpful,” citing situations where a patient has their first DBT exam after “years of 2D digital mammograms, where you’re seeing what looks like new distortion. When the patient is called back for reimaging, we find there was a scar there. So subtle, the tech didn’t even see it.”
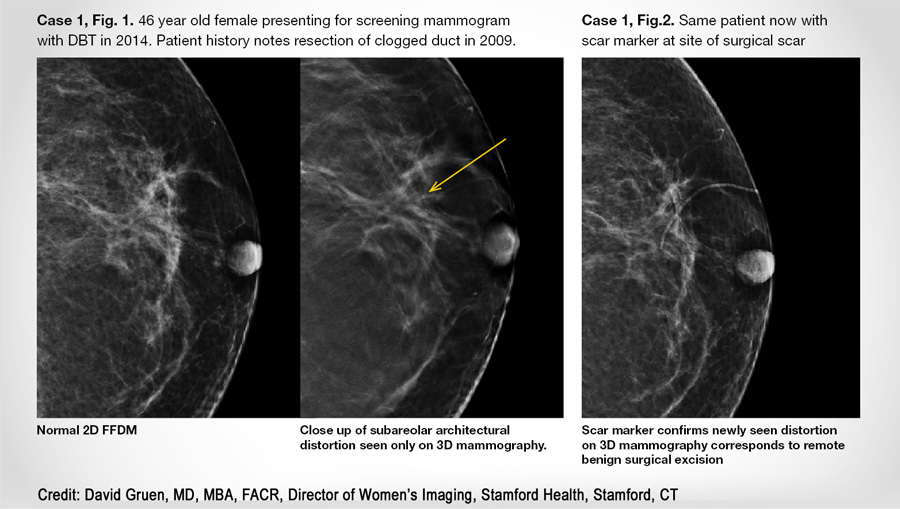 Scar markers help to correlate the new architectural distortion seen within the parenchyma to a historical event. As such, these radiologists depend heavily on their technologists to provide them with that documentation of previous surgical sites and other observations seen on the patient’s skin.
Scar markers help to correlate the new architectural distortion seen within the parenchyma to a historical event. As such, these radiologists depend heavily on their technologists to provide them with that documentation of previous surgical sites and other observations seen on the patient’s skin.
The crucial role of the technologist in communicating and documenting critical observations
“Technologists are extremely important in screening mammography because we don’t ever see that patient,” stated Robert Meli, MD (ProScan Imaging, Naples, FL). “They’re the ones who see dimpling or anything, really, that can raise questions later on. So, we rely heavily on them to communicate what they observe, which is essential as we don’t see those surface details on the screen.”
By using all the tools at their disposal - open communication between physician, technologist, and patient, known patient history, and marking of all post-surgical scars can help breast imaging facilities improve accuracy and reduce questions regarding architectural distortion seen on DBT that can lead to unnecessary additional workups.
Learn more:
To learn more about the benefits of skin markers for permanent documentation of communication in mammography, contact your Beekley Medical Account Specialist at 1-800-233-5539 or info@beekley.com to learn more.
*Names of these panelists were withheld in compliance with employer policy
Related articles:

Kathy Kaschuluk
Product Manager
