
Although the onus of interpretation lies on the radiologist - mammographers are on the front lines when it comes to patient care and clinical efficacy. From positioning to communication to documentation, they can represent the difference between a caught or missed cancer.
In her article “Importance of Visual Checks Before Mammograms,” educator and author Olive Peart, M.S., RT (R)(M), notes that the mammographer is “most often the only link between the radiologist and the patient. The information the mammographer does or does not convey can aid in diagnosis and action or lack of action can have repercussions.”
Communication is key for the patient experience and radiologist's image interpretation
With that in mind, Ms. Peart summarizes that communication is key to both the patient experience and the radiologist’s image interpretation.
As the patient liaison, face to face communication between the mammographer and the patient is a necessity – not only to gain the patient’s family or personal history with breast cancer, but also as an opportunity to help educate the patient, alleviate her fear or anxiety, and clarify any misconceptions she may have.
This data includes visual checks for the following which may be, or may be interpreted as, signs of breast cancer:
- Skin thickening
- Unusual lumps
- Moles and other skin lesions
- Accessory nipple/breast tissue
- Nipple changes
Documenting and communicating patient's clinical information
In addition to capturing this information on the clinical history form, it makes sense to have documentation on the skin as well.
As Ms. Pert points out, “The clinical history sheet may or may not travel with the patient’s images if she goes elsewhere for treatment.” Physical documentation with mammographic skin markers provides lasting visible clinical documentation.
However, not every facility, or every radiologist, speaks the same language when it comes to documentation with skin markers.
Ms. Peart references reports of false-negative interpretation due to non-standardized marking systems in her article and cites a case where a mammographer used a “BB” to indicate a palpable lump as was the protocol, and the radiologist, who was new to this facility, interpreted it as a skin lesion, as that was the practice at her prior institution.
A universal, standardized protocol helps prevent miscommunication and errors
She goes on to state that improving standardization can lead to fewer misinterpretations with their resultant lawsuits, and reduce confusion when patients go to different facilities.
The ACR now recommends in their Practice Parameters for Screening and Diagnostic Mammography that facilities require "consistent use of radiographically distinct markers to indicate palpable areas of concern, skin lesions, and post-surgical scars," yet fall short of recommending standardization of the type of marker used for each of the above areas.
However, we are seeing signs of self-standardization of communication among skin marker vendors and breast imaging facilities that mark: linear markers indicate post-surgical scars, circular markers communicate raised moles or skin lesions, pellet or “BB” markers identify nipple location, and triangular markers communicate palpable findings.
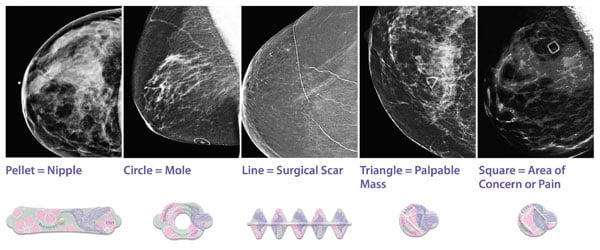
In order to reduce any chance of confusion or miscommunication, Beekley Medical introduced a square marker for communicating a focal point of pain or any non-palpable finding area that may image such as cysts, bug bites, bruising, or ecchymosis.
Ms. Peart states that “In addition to performing the actual mammogram, the mammographer needs to be a compassionate and skilled communicator.” Visual checks and a standardized skin marking system in mammography are an important extension of that compassion and communication.
To learn more about the role mammographic skin markers play in clearly communicating vital information to the interpreting radiologist, contact your Beekley Medical Account Manager at 1-800-233-5539 of info@beekley.com.
Related articles:

Mary Lang Pelton
Director of Marketing Communications
