
In the early days of radiation therapy, two-dimensional X-ray images and manual mathematic calculations were utilized to create treatment plans. In the 1970’s, the advent of computerized systems improved dose accuracy and the increased application of the Monte Carole (MC) problem solving method increased the speed of dose calculations.
Technology enables planning for targeted, more precise, radiation dose
Today, the practice of 3-D radiation therapy is performed by a team of health care professionals consisting of radiation oncologists, medical physicists, medical dosimetrists, and radiation therapists, who work together to plan the appropriate treatment for a patient with cancer.
 This team makes use of high-tech machines with sophisticated software that allows them to deliver concentrated radiation therapy to a very targeted location within the patient’s body.
This team makes use of high-tech machines with sophisticated software that allows them to deliver concentrated radiation therapy to a very targeted location within the patient’s body.
These technological advancements, along with the widespread increase in the use of the MC method in radiotherapy dosimetry calculations, has led to more targeted treatments and better patient outcomes.
But regardless of these technological innovations, issues can still arise with regard to the precision of the treatment plan due to the concern of dose perturbation caused by skin markers used during CT simulation.
Prior to the creation of a patient’s radiotherapy treatment, radiation therapists employ a variety of tools that help to ensure the accuracy of the targeted radiotherapy such as immobilization devices, lasers, and linear skin markers. The skin markers are used in treatment planning to outline field borders and mark tangents, scars, sarcomas and larger treatment areas.
Dose perturbation - a speed bump on the road to precise treatment planning
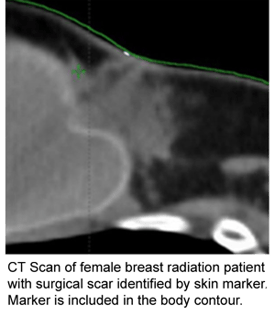
Because linear skin markers lie on the skin, they are included inside the automatic body contour established at the start of treatment planning. When the planning algorithm calculates radiation treatment dose, it considers the density of the linear marker in the plan.
So, in order to avoid over-dosage, the dosimetrist must manually contour the skin marker and assign it a density of zero or 1 depending on their type of plan. If the dosimetrist does not manually contour the marker and override the density, there can be instances of dose perturbation.
This is a tedious, time consuming process. Unfortunately, automatic and manual contouring can also be imperfect and lead to dose inaccuracies.
An innovative new linear marker minimizes dose perturbation
Any discrepancies will lead to the request for a rework of the treatment plan by the physicist or oncologist, adding more work for the dosimetrist and possibly delaying the patient treatment.
RT-SPOT®, Beekley Medical's newest skin marker for radiation oncology, is elevated from the skin line on a unique, radiolucent foam backing. By raising the imaging portion of the linear marker away from the skin line keeps it outside the automatic body contour.
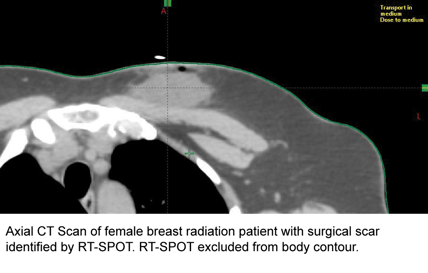
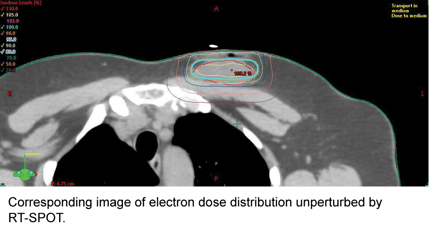
With RT-SPOT, planning  software will not consider the marker’s density when calculating dose and the dosimetrist will not have to take the extra step of manually contouring or overriding the marker’s density. This helps to improve workflow, save time, decrease the need to rework a treatment plan, and increase accuracy.
software will not consider the marker’s density when calculating dose and the dosimetrist will not have to take the extra step of manually contouring or overriding the marker’s density. This helps to improve workflow, save time, decrease the need to rework a treatment plan, and increase accuracy.
To learn more about RT SPOT, contact your Radiation Oncology Account Manager at 1.800.233.5539 or email info@beekley.com.
Related articles:

Beth Kyle
Product Manager
