With October being Breast Cancer Awareness Month, we thought we would shed some light on mammograms and how vital they can be in detecting cancers, as well as what to expect when you schedule your first mammogram.
Mammograms save lives
“Mammography is an early-detection tool, if we do find something, it’s usually in the early stages and helps give patients the best outcome” according to Jenny Ton, mammography technologist at Cedars-Sinai. Catching breast cancer at an early stage is crucial. It gives the patient more treatment options and a better chance of survival Jenny added.
The American Cancer Society states that a mammogram can often find breast changes that could be cancer years before physical symptoms develop and results from many decades of research clearly show that women who have regular mammograms are more likely to have their breast cancer found early, are less likely to need aggressive treatment like surgery to remove the breast (mastectomy) and chemotherapy, and are more likely to be cured.
About the procedure
It is recommended that women 40 and over should get an annual mammogram but it is never too late to start. Once you arrive at your appointment, check in, and get into the exam room, you will be asked to undress from the waist up and will be provided a gown for your comfort.
Next, the technologist will examine your breasts, looking for any skin changes or puckering. During this time, they may also place markers on your skin to signify important landmarks for the radiologist such as any moles, surgical scars, and nipple location. There are also special markers for lumps felt during a physical exam, points of pain, or other non-palpable areas of concern.
 The technologist (the person who performs your mammogram) will then manually position your breast in the machine for each image, making sure both your breast and body are in the correct position. Your breast will be between two plates that will be applying pressure while the imaging takes place, which only takes approximately 10 seconds. You may also be asked to hold your breath during this time so that there is no motion during the image-taking procedure.
The technologist (the person who performs your mammogram) will then manually position your breast in the machine for each image, making sure both your breast and body are in the correct position. Your breast will be between two plates that will be applying pressure while the imaging takes place, which only takes approximately 10 seconds. You may also be asked to hold your breath during this time so that there is no motion during the image-taking procedure.
"It can be uncomfortable, but we need to apply the pressure to spread out the tissue so that we get a clearer image of the breast tissue," says Jenny. "The more pressure that is applied, the less radiation will be needed to get an optimal image."
After the technologist gets all the images they need, usually two of each breast, you will be able to leave shortly after. It will usually take no more than two weeks to receive your results.
Many mammography centers use receptor plate covers to help make positioning easier for the technologist so that she can get as much tissue imaged as possible and help make process more comfortable for the patient – especially those patients with thin skin or who tend to stick to the receptor plate after being released from compression.
Some women may require additional imaging or get called back for a follow-up mammogram. Getting called back is more common after a first mammogram, or when there’s no previous mammogram to compare the new mammogram to. It's also more common in women who haven’t gone through menopause.
Helping to prevent unnecessary callbacks
“When your diagnosis must be right®” isn’t just a tagline or slogan for Beekley Medical, especially when it comes to breast cancer screening and detection.
In fact, Beekley Medical pioneered the idea of a shape communication system for mammography - a system of distinctly shaped skin markers that help reduce questions that can lead to additional imaging, missed diagnoses, or even misdiagnoses.
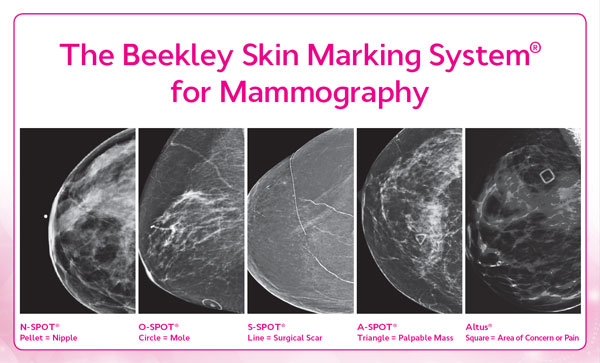 These mammography skin markers identify and permanently document the location of nipples, skin scars, moles, palpable masses, and any other areas of concern on the mammographic image for the radiologist – making it easy to compare your images from year to year and note any subtle changes that could affect your breast health.
These mammography skin markers identify and permanently document the location of nipples, skin scars, moles, palpable masses, and any other areas of concern on the mammographic image for the radiologist – making it easy to compare your images from year to year and note any subtle changes that could affect your breast health.
As an example - if you have a raised mole on your breast, the circular skin marker (the shape that indicates a mole) will be placed around your mole. The radiologist sees the circle and automatically knows that what they are seeing is a mole on the skin.
Why is this important? Because moles can sometimes look like a cancer. By marking the mole year after year, the radiologist will know that it is not a cancer or an area requiring further workup or additional imaging.
A mammogram is nothing to stress over, even during COVID-19
The entire procedure takes approximately 15 minutes – less time than you would spend in the grocery store. So, don’t let fear of the exam or the virus keep you from getting this important exam.
Imaging facilities are doing their utmost to keep you and their staff safe from contracting COVID-19. Equipment and dressing rooms are disinfected after every patient, temperature checks, mandatory masking, and social distancing measures are put in place for both patients and staff.
If you are nervous, ask your breast center if they offer any relaxation tools such as clinical aromatherapy to help soothe and calm you during the exam. If they don’t provide any, you can purchase your own from the consumer shop at Elequil.com to bring with you.
Remember early detection saves lives!
Related articles:

Megan Sargalski
Marketing Communications Specialist
