Pink ribbon season is almost here. Yet, despite all the millions spent on breast cancer awareness, women are still reluctant to go for annual screening mammography. And when they do go, many see it as an unpleasant task rather than an important step in their personal fight against breast cancer.
It almost seems as though breast cancer awareness campaigns are victims of success as women seem more educated about the marketing aspect of breast cancer awareness (football, yogurt lids, clothing, jewelry, and more) than about the actual exam that could one day save their lives.
The messages to donate to the cause or to participate in fun functions for the cause come through loud and clear, but somehow the communication about the single most important step to combat mortality from this disease has gotten muddled.
Perhaps it's time to talk about "Mammography Awareness" and clear up the misconceptions surrounding this life-saving exam.
Where to begin? Perhaps the biggest, and most potentially harmful, blow came in 2009 when the U.S. Preventative Services Task Force (USPSTF) revised its recommended screening guidelines for breast cancer.
The revisions (made without a single member on the task force with expertise in the diagnosing or treatment of breast cancer) recommended that first mammograms begin at age 50 instead of 40 and then screening mammograms every two years instead of every one.
As a result, the number of women going for mammograms dropped by an average of 9% across all demographics in the 3 years following the announcement. Even though these guidelines were somewhat revised, many women and the referring physicians remain confused about when to start screening mammography and how frequently they should go.

While the American Cancer Society and the Centers for Disease Control also modified their screening guidelines to reflect that of the USPSTF, the groups on the front lines of early detection such as the American College of Radiology, The Society of Breast Imaging, and The National Consortium of Breast Care Centers all stand by the old guidelines of annual mammograms beginning at 40 (with assessments even earlier for women in high risk groups) as it has been proven to catch cancers in earlier stages and lower mortality rates.
Why are women staying away?
I think it's safe to boil it down to fear of the two "C's" - compression and cancer. Let's face it, it's not the most pleasant exam to endure and the whole reason we are there is to see if we have a cancer lurking in our brassieres. It's no wonder so many women looked at the USPSTF guidelines as an excuse to put off the perceived physical and potential emotional discomfort for as long as possible.
And if it isn't fear of a cancer already there, there are a few "urban myths" out there that the exam itself puts one at risk.
Urban myths that need busting in breast imaging:
One of the more recent, and stubbornly persistent, is the claim that radiation from the exam can cause cancer of the thyroid. The American Thyroid Association (ATA) itself states, "With regards to mammography, the ATA does not recommend thyroid shields for mammography due to a lack of data to substantiate their use and the extremely low amount of radiation that reaches the thyroid. Furthermore, any risk to the thyroid is much lower than the benefit of mammography."
 But, because this claim originated with a TV celebrity, it gained credibility very quickly, prompting concerns that this was yet another excuse for women to put off their mammograms and necessitating responses from imaging professionals as to how the use of a thyroid shield can actually interfere with the mammography exam and actually lead to more radiation exposure.
But, because this claim originated with a TV celebrity, it gained credibility very quickly, prompting concerns that this was yet another excuse for women to put off their mammograms and necessitating responses from imaging professionals as to how the use of a thyroid shield can actually interfere with the mammography exam and actually lead to more radiation exposure.
An older myth is that the radiation from the exam increases the risk of breast cancer. While it's true that mammography involves radiation, the exposure is significantly less than the every-day background radiation we are exposed to on earth. The benefits of mammography far outweigh the perceived risks.
Another misconception derives from the fact that breast imaging has gotten better at detecting cancers at its earliest stages. As a result, radiologists are seeing more detail in breast tissue that could be precursors to breast cancer and referring women for additional procedures to confirm or rule out a cancer diagnosis. This might mean additional images under mammography, or another imaging modality such as ultrasound or MRI or, it might mean a biopsy procedure for tissue samples to be sent to pathology for a definitive answer.
The good news is most findings are benign and life goes on as usual. Where most (I hope) would find this type of due diligence a good thing when it comes to one's health, it's easy to find words like "over-diagnosis" and "unnecessary treatment" screaming from headlines about one study or another.
What gets lost from the messaging is that cancer is unpredictable and early signs don't always signal their intent as to whether they're aggressive or essentially harmless from one woman to the next.
So, how can breast imaging providers overcome these misconceptions and get women in for their annual screening mammograms?
It may seem like an over-the-top metaphor, but breast imaging professionals are in a battle for the hearts and minds of our consumers. And the best way to win them over is through empathy, communication, education, and accommodation.
 Empathize: It's easy to let the exam become rote when you've done it so many times, but for the patient it is anything but rote. She comes to you with reluctance, fears, and/or memories of previous mammograms - particularly ones that were not so pleasant.
Empathize: It's easy to let the exam become rote when you've done it so many times, but for the patient it is anything but rote. She comes to you with reluctance, fears, and/or memories of previous mammograms - particularly ones that were not so pleasant.
The article "The Mammogram Assault! It Doesn’t Have to Happen to You!" by Kathleen Reardon, breast cancer survivor, Professor Emerita, University of Southern California Marshall School, and contributor to the Huffington Post, is a great read about how the lack of empathy exhibited during the mammogram experience can ruin trust in you as a provider and in the exam itself.
Ms. Reardon describes her experience with a particular technologist as cold, unfeeling, impersonal: "The technician didn’t walk with me, as several others had done in years past, smiling and endeavoring to relax me. No, she was gone, and I wandered the hallway to find the right room. There was no time for small talk, just a few questions about my history and then we got started - my birth date, doctor’s name and my own. Missing was a gentle touch on my shoulder as some technicians had ventured in previous years. Absent was any assurance that 'This won’t take long' or 'Tell me right away if this hurts too much.'"
She goes on to describe the callous indifference shown to her during the exam when she cried out in pain under compression of her sensitive and radiation-scarred breast and sums up her article stating that "Mammography, as is common with MRIs, should be done with compassion. 'Would you like to rest between views?' and 'We have one more to do. How are you feeling?' are the kinds of questions mammography patients need to hear."
"Bedside manner" goes a long way in breast imaging.
Communicate: If you want to drive screening compliance and lower no-shows, send reminders.
According to one study, among women who recalled receiving reminder letters and either made an appointment or went for their mammograms, 74.8% (122 of 163) indicated that the letters substantially influenced their decisions. Most respondents 77.1% (296 of 384) indicated that they would like to continue to receive reminders, and 28.9% (111 of 384) indicated that they would like to receive additional information about mammograms.
Another study examined text messaging reminders and found a 23% reduction in non-attendance rate after the implementation of text message reminders.
We all lead busy lives and it's easy to "keep forgetting" and put off doing something we don't really want to do in the first place. Reminders help keep us accountable to ourselves.
 Educate: Take advantage of educating your patients at every touch point. Most imaging facilities have great websites explaining the exam and answering patient concerns.
Educate: Take advantage of educating your patients at every touch point. Most imaging facilities have great websites explaining the exam and answering patient concerns.
But perhaps that same information should be available in your reminder letters, and throughout the breast imaging center. Patient-friendly posted information in waiting areas, dressing rooms, and the exam room get noticed and read.
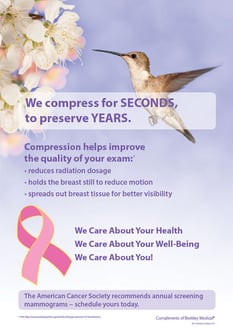
Beekley Medical can even help you get started with a free library of educational mini-posters that help explain the exam, compression, and why certain products like skin markers and receptor plate covers are used during their mammogram
Many facilities host an open house when they get a new piece of equipment or remodel, but why stop there? How many women become eligible for their first mammogram or move into your community each year?
What better way to alleviate concerns and encourage women to choose your facility by encouraging them to tour you facility, meet your staff, ask questions, learn about the machines and the procedures as demonstrated in this example from Women's Imaging Center at Memorial Hospital Miramar .
Accommodate: Tying into empathy is accommodation. If we understand what makes women anxious about their mammography exam, we can be proactive in making it a more comfortable experience.
Many facilities have implemented evening and weekend hours to accommodate busy schedules. Some have rapid review of images to reduce waiting time for results.
Breast centers are being redesigned with spa-like elements such as neutral tones, water sculptures, comfy chairs, and serene music to help create a calming environment while patients are waiting for the exam.
You can also take advantage of tools that are designed for improving both clinical efficacy and the patient experience.
Designed with both you and your patient in mind
Aside from their clinical advantages, Beekley SPOT® mammography skin markers and receptor plate covers such as Bella Blankets® help improve patient perception of the exam.
The regular and consistent use of skin markers to indicate topical landmarks, prior surgical sites, and palpable or non-palpable areas of concern can help reduce unnecessary additional imaging to confirm or rule out a suspicious finding. If a patient comes in with a complaint or has been called back repeatedly because a mole imaged oddly, the placement of the skin marker - and the explanation that the marker will alert the radiologist that this is the lump she felt, this is the mole - will let the patient know you heard her.
In addition to helping capture more breast tissue, Bella Blankets also helps with patient perception by providing a more comfortable surface than a bare receptor plate and helping to prevent breasts from sticking to the plate and potential skin tears.
Elequil aromatabs® enhance the patient experience through the use of 100% essential oils to help reduce anxiousness. An independent 4-year clinical study showed that inhalation aromatherapy with lavender-sandalwood Elequil aromatabs significantly reduced self-reported anxiety in patients undergoing breast biopsy procedures.
 The more we can do to encourage women to know more about the benefits of annual screening mammography and make it as positive an experience as possible when they are in our facilities, the better we can counteract all the confusion and misconception out there.
The more we can do to encourage women to know more about the benefits of annual screening mammography and make it as positive an experience as possible when they are in our facilities, the better we can counteract all the confusion and misconception out there.
Consider Beekley Medical your partner in patient care and feel free to reach out to us as to how we can help you overcome patient avoidance of screening mammography at your facility.
Related articles:

Mary Lang Pelton
Director of Marketing Communications
