Since first suggested in 1976, CT guidance during interventional procedures has become indispensable. Common procedures that utilize CT guidance and can benefit from a localization device include biopsies, drainages, cryoablation, celiac plexus, and other pain management blocks.
As with any procedure involving ionizing radiation, it is desirable to perform the procedure with the least amount of radiation to the patient as well as minimize discomfort and adverse outcomes.
These procedures can be divided into three phases: the planning phase, the actual procedure itself and the post procedure monitoring of the patient.
Planning for first-stick success, minimal radiation
During the planning phase, the previously obtained diagnostic CT will reveal the location of the target. A scout and planning slices are obtained, and the ideal slice, needle entry site, and trajectory of the needle will need to be determined.
In some cases, due to the superficial nature of the target or the presence of obvious anatomical structures, localization of the needle entry site can be determined without help. For all other cases, the use of a localization device on the skin surface is helpful, and in many cases - where the target is small, deep, and next to critical structures - it is vital.
Accurate determination of the needle entry site can lead to first stick success, minimizing second passes of the needle or sheath as well as limiting the need for additional imaging.
Many studies have shown that adverse outcomes can increase with the number of attempts or passes of the needle.
A coaxial technique can allow for multiple samples through a single puncture, but placement of the sheath is still dependent on accurate puncture site planning.
Regarding lung biopsies, the incidence of pneumothorax (approx. 20-23%) was related to increased pleural passes.1,2
Similarly, Cadranel et. al. found that the incidence of complications in percutaneous liver biopsies also increased with the number of passes. They found that the frequency of complications was 26.6% with one pass and increased to 68% with two or more passes.3
Reduction of radiation dose during the planning stage is particularly important, as most of the overall dose of the procedure occurs during this phase. 90% of the total dose is delivered in the helical planning stage during CT fluoroscopy.4
Park et. al. found that the highest dose received by the patient during CT guided cryoablation also occurred during the planning phase.5
To that end, it is important that whatever method you use to locate the needle entry site, it does not contribute to increased dose of radiation and is as accurate as possible to minimize second passes of the needle.
Use of a single pellet
Numerous studies cite the use of a grid to determine the needle entry site1,4,5,6, but we still hear about the use of older methods being used today.
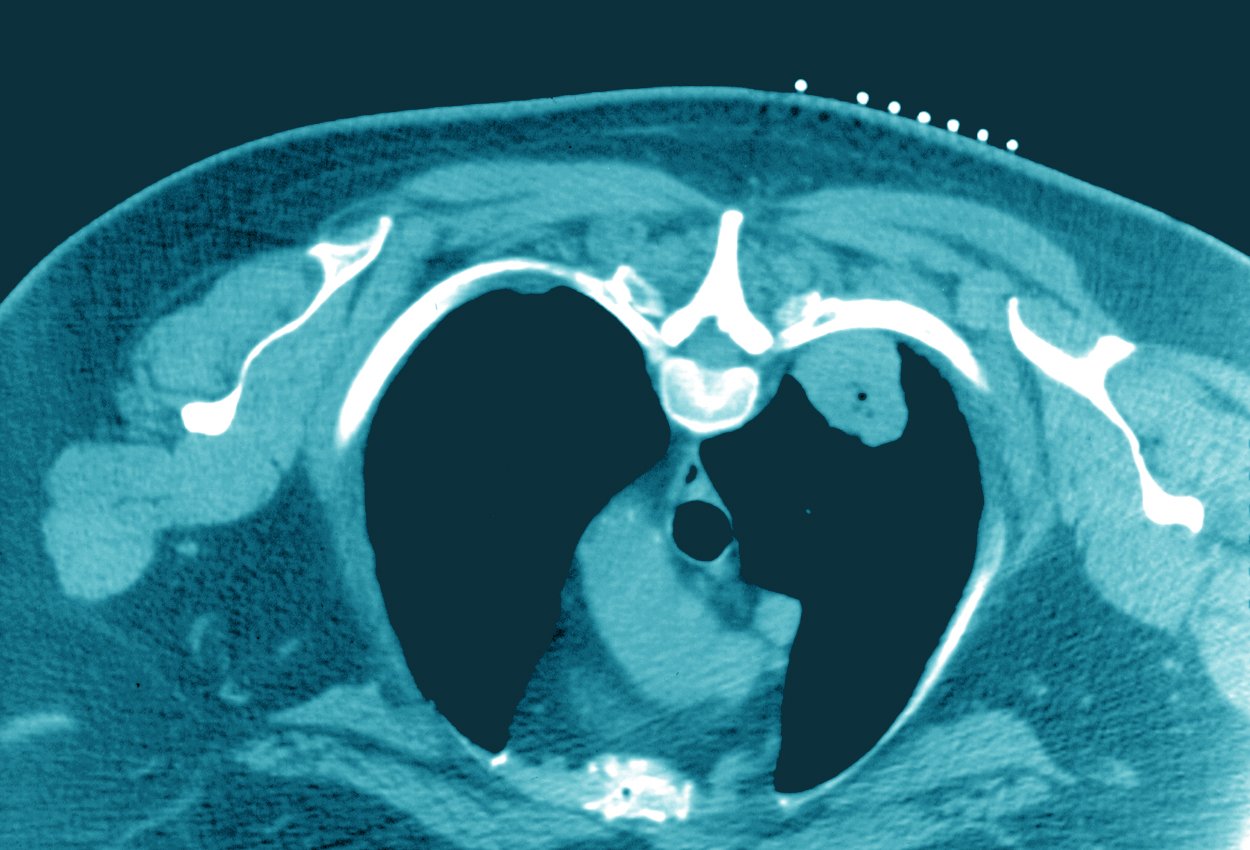
The use of a single pellet as your landmark can pose several challenges. If the pellet is not placed in the exact location of the ideal needle entry site you are forced to either move the marker and scan again or measure from the current location.4 (See Image 1)

Image 1: The ideal needle entry site is a significant distance from the fiducial marker.
Additionally, whenever respiratory motion is a factor, the patient will need to exactly replicate the breath hold they performed before the pellet was placed, and again after placement when the slice is acquired to capture the image of the pellet. If the patient “breathes off the mark,” then the slice or slices will need to be repeated which adds to the planning dose total.
Use of a "makeshift" grid
Makeshift grids made from expired catheters also have significant drawbacks.
At times, the source of your catheters may not have expired catheters to give, and even if they do, the grids need to be cut and assembled. Building multiple grids can be time consuming and takes technologists away from actual patient care. Additionally, makeshift grids will not have uniform spacing and will not conform to the curves of the body, leading to planning inaccuracy. Of course, reusing any product for this purpose also raises infection control issues.
Why professional grids are the ideal device for localizing needle entry points
The ideal device for localization of the needle entry site during CT guided procedures is a grid that conforms well to the contours of the body and images in a consistent manner without artifact.
When using a professional grid for CT-guided interventions, you can determine the location of the target from the diagnostic CT. This allows you to place the grid over the target prior to the scout or planning slices. As discussed earlier, when using a single pellet, you would need to scan prior to the placement of the pellet and then after placement to capture the pellet on the chosen slice. A patient cannot “breathe off the mark” when using a grid.
It is also helpful to have choices when determining the ideal approach to a lesion.
The use of a professional grid gives the practitioner those options. A larger grid is useful in special situations - for example those including bariatric patients or when there are two or more lesions to sample. Celiac plexus blocks performed for intractable abdominal pain, typically from pancreatic cancer, are performed on each side of the vertebral column. During the planning phase, the use of either two smaller grids (Image 2) on each side of the spine or one larger grid will result in the need for just one scan to plan the procedure.5
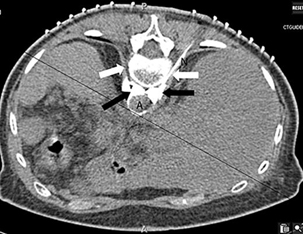
Image 2: Two grids being used to plan a celiac plexus block. N= needle.
Cryoablation, which utilizes several probes to create an ice ball within cancerous lesions using a freeze/thaw cycle also utilizes CT guidance during the planning phase. Due to the need to place multiple probes, a grid placed over the organ of interest can facilitate the ideal localization with the least amount of dose to the patient.
Beekley Medical has created GuideLines®, a product family of three different grids that accomplish all of the outcomes outlined above. Two of the grids have windows to access the skin between the lines while the third grid enables the physician to mark directly through the grid. The grid lines are composed of a non-metallic material to minimize beam hardening artifact. And most importantly, all Beekley Medical grids have a fully adhesive backing to ensure that the grid contours to the body leaving no room for error.
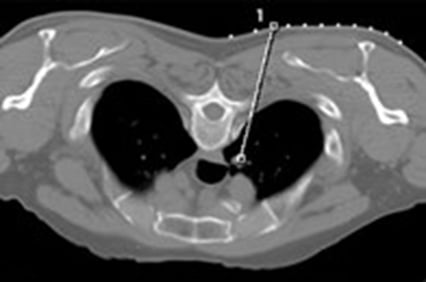
Image 3
If you would like to see more first-stick accuracy and reduced radiation dose to your patient during CT guided intervention planning, ask about a trial evaluation of GuideLines® biopsy grids to compare to your current method. Contact your Beekley Medical Business Development Manager at 1-800-233-5539 (+1-860-583-4700) or email info@beekley.com.
For product safety information, visit www.beekley.com
References
- Cadranel, J. , Rufat, P. and Degos, F. (2000), Practices of Liver Biopsy in France: Results of a Prospective Nationwide Survey. Hepatology, 32: 477-481. doi:10.1053/jhep.2000.16602
- Sarti M, Brehmer W, and Gay S, Low-Dose Techniques in CT-guided Interventions. RadioGraphics 2012 32:4, 1109-1119
- Park B, Morrison P, Tatli S, et al. Estimated effective dose of CT Guided percutaneous cryoablation of liver tumors. Euro J Rad. 2011. 04.06
- Gruber-Rouh T, Thalhammer A, Klingebiel T, et al. Computed tomography-guided biopsies in children: accuracy, efficiency and dose usage. Ital J Pediatr. 2017;43(1):4. Published 2017 Jan 6.10.1186/s13052-016-0319-7.
Related articles:

Richard Foster
Director of Training
