What makes for an "aha" moment?
For Dr. David Gruen, Director of Women's Imaging for Stamford Health (Stamford, CT), it was the realization that he and his team were working up more patients for architectural distortion in 3D Mammography (Digital breast tomosynthesis or DBT) that ultimately turned out to be associated with scarring from benign excisions from surgeries performed several years earlier.
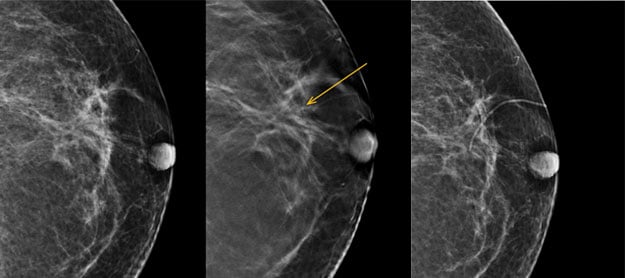
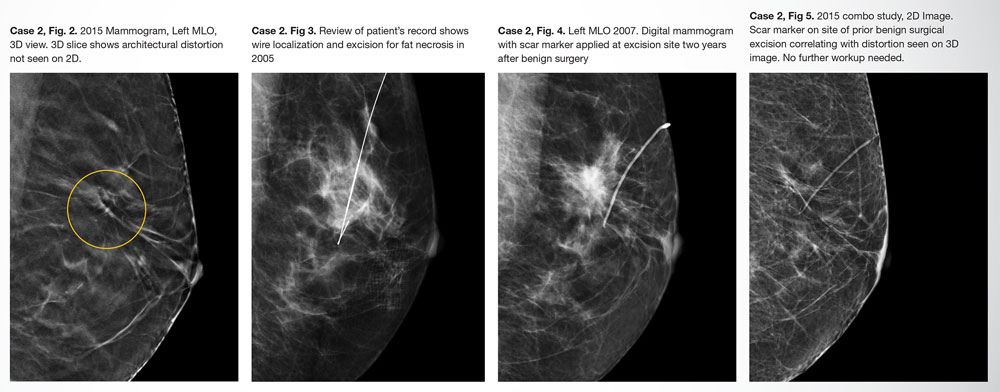
As he explains in his paper, "Benign Intraparenchymal Scarring in the DBT Era," before 3D mammography,intraparenchymal scarring seemed to go away as the lumpectomy bed healed and changes in the breast stopped being visualized. The skin scar itself became difficult to see and it didn't seem necessary to continue to mark it.
With digital breast tomosynthesis, however, radiologists are seeing architectural distortion from surgeries that hadn't been seen in years under 2D imaging.
In Dr. Gruen's experience, it wasn't uncommon to go back and look at a mammogram from 5 years prior, sometimes even 10, to see a scar marker in both projections with the architectural distortion seen seen on DBT right at the crosshair and then going back another 2 years to see that it was indeed where the wire localization and prior surgery had taken place.
"We may not have focused on benign intraparenchymal scarring in the 2D era, but it is obvious that we see it frequently in the DBT era, so marking all scars is significantly more important."
According to Dr. Gruen, since the skin scar is the only externally visible mark of a surgical excision, it is important to mark those scars to discern whether the architectural distortion seen in 3D mammography is from a prior surgery rather than an indication of a new cancer.
"In breast imaging, the clinical imperative is breast cancer."
As Dr. Gruen put it - If someone has an architectural distortion, they're going to be worked up. If it cannot be attributed to a previous benign surgery, then they'll wind up being biopsied to determine if it's cancer or not. Because DBT finds so many more areas of architectural distortion,he advises that radiologists use all the tools at their disposal to ensure more accuracy with intraparenchymal scarring. These tools include:
- Open communication between physician, technologist, and patient
- Known patient history
- Marking all post-surgical scars

About David Gruen, MD, MBA, FACR
Dr. David Gruen is fellowship-trained in Oncologic Imaging with an expertise in breast and body imaging. He is a nationally regarded expert and consultant on all aspects of breast radiology. Dr. Gruen is the first diagnostic radiologist in the United Sates to be appointed as an inspector for the National Accreditation Program for Breast Centers (NAPBC) and serves as a member of the Connecticut Hospital Association task force on radiation safety.
Acknowledgement:
Because of the high volume of DBT exams performed, the Tully Breast Imaging Center at Stamford Health served as a test site to evaluate the radiopacity and minimization of artifact of various prototypes during the development of Beekley Medical's TomoSPOT® skin markers for 3D digital breast tomosynthesis.
Learn more about Dr. Gruen's "aha" moment and the cases that brought him full circle back to marking scars by clicking the thumbnail of the paper "Benign Intraparenchymal Scarring in the DBT Era" below:
Related articles:

Mary Lang Pelton
Director of Marketing Communications