Two of the exams used in the diagnosis of abdominal diseases include a routine CAT-Scan (CT) of the abdomen and pelvis, and small bowel enterography which can be performed in either CT or MRI.
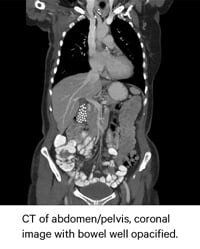 A routine CT of the abdomen and pelvis can help diagnose problems in the bladder, uterus, or prostate; liver or bowel abscesses in the abdomen, inflamed colon; cancers of the colon, liver, pancreas, and kidneys; pancreatitis; diverticulitis; appendicitis; lymphoma; and staging for cancer.
A routine CT of the abdomen and pelvis can help diagnose problems in the bladder, uterus, or prostate; liver or bowel abscesses in the abdomen, inflamed colon; cancers of the colon, liver, pancreas, and kidneys; pancreatitis; diverticulitis; appendicitis; lymphoma; and staging for cancer.
Enterography in CT or MRI can be used to differentiate and evaluate the organs of the abdomen and pelvis but its primary function is in the evaluation of diseases of the small bowel, specifically in patients with suspected or known Crohn’s disease.
Optimal image necessary for accurate diagnosis
In both exams, the hallmarks of a good study are proper positioning, perfect imaging technique, and a successful prep.
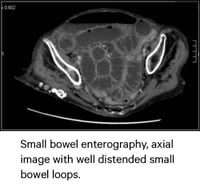 Preparation for the exam includes fasting prior to the exam, the administration of oral contrast, and the use of IV contrast at the time of imaging.
Preparation for the exam includes fasting prior to the exam, the administration of oral contrast, and the use of IV contrast at the time of imaging.
The oral and IV contrast help to differentiate between the bowel and other organs, and help to identify pathology, bowel obstructions, as well as bowel perforations.
In enterography, the neutral oral agent provides good lumen visualization, and more importantly, distention of the small bowel - especially within the terminal ileum.
Palatability: the difference between an optimal image and a repeat exam or NG tube
As most imaging facilities are aware, there is a major obstacle to obtaining an optimal scan in both of these exams for diagnosing abdominal diseases: the patient’s ability or, more accurately, their inability to drink and tolerate a large volume of liquid.
Though the contrast media is different for routine CT of the abdomen and enterography; taste or palatability remains the greatest complaint from patients undergoing these studies.
Facilities that use iodinated contrasts such as Gastrografin® or Gastroview® for routine CT of the abdomen are familiar with the associated bitter metallic taste.
Patients, many of whom are sick to begin with, struggle to drink the required 900-1000 ml of this bitter liquid.
Technologists and physicians may explain to the patient how leaving the contrast drink unfinished can result in a poorly opacified bowel which can result in a non-diagnostic exam. But, despite this coaching, the experience will still be unpleasant and some patients will be unable to finish the entire volume of fluid necessary for their scan,
Neutral distending agents used in enterography have a thick consistency and have historically not tasted good.
Because distention is the end goal, patients are typically asked to drink between 1000 -1500 ml of the neutral agent. This volume can be a problem for patients, which is compounded by the poor taste and the viscous texture.
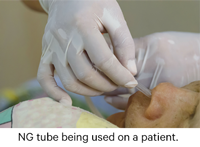 The difficulty to drink can be so severe, that facilities may need to resort to other measures. Donna Pflugg, CT Supervisor for the Children’s Hospital of Pittsburgh told us that because the contrast agent used for enterography was slimy, many of her patients simply could not tolerate it, and as a result, “A lot of patients had to get an NG tube.”
The difficulty to drink can be so severe, that facilities may need to resort to other measures. Donna Pflugg, CT Supervisor for the Children’s Hospital of Pittsburgh told us that because the contrast agent used for enterography was slimy, many of her patients simply could not tolerate it, and as a result, “A lot of patients had to get an NG tube.”
So if both exams rely on the patient drinking a large volume of oral contrast for a successful exam, what can imaging facilities do to overcome the obstacles of taste and palatability?
Working around the taste / texture
There are some facilities that choose not to use contrast for the sake of time and cost. Of course, this can be problematic as there is always the risk of an unsuccessful exam that may need to be repeated.
However, most facilities strive to create a better taste experience for their patient in the attempt to achieve greater compliance with drinking instructions - particularly for the bitter contrast used in routine CT of the abdomen.
In order to mask the taste, facilities have used a variety of commercial beverages with powdered drink mixes such as Kool-Aid® or Crystal Lite® or they mix the contrast with another beverage of choice. Many patients can testify how ineffective these methods are.
Wayne Dixon, a 73-year-old patient in Maryland was not looking forward to his second abdominal CT scan after his first experience. He told us, “It was not a pleasant experience. They mixed the contrast with Crystal Lite for my first exam. I could not tolerate the taste. I would never want to repeat that experience.”
In enterography exams, radiologists may choose not use any commercial agent and just use water alone to distend the bowels.
However, a study from the Mayo Clinic found water to be one of the least effective distending agents for enterography as water is rapidly absorbed by the small bowel mucosa.
Two exams. One goal. Two Solutions to improve palatability and drinking compliance
The Breeza® family of flavored beverages for abdominal imaging was created by a radiologist determined to overcome the challenges patient were having with drinking compliance as they prepped for their exams.
Breeza® flavored beverage for use with oral iodinated contrast (REF 220) was designed to solve the taste problem of oral iodinated contrast.
 This sugar-free and gluten-free, tropical fruit- flavored beverage was specifically designed with a bitterness blocker to improve the taste and palatability of the oral iodinated contrast.
This sugar-free and gluten-free, tropical fruit- flavored beverage was specifically designed with a bitterness blocker to improve the taste and palatability of the oral iodinated contrast.
On his second CT -Scan, Wayne Dixon was given contrast mixed with Breeza 220. He said that “Without a doubt, Breeza 220 made a world of difference for my exam. I had absolutely no trouble drinking this at all. I drank both bottles within the required one hour and had no side effects, nothing. The taste is very pleasant unlike the Crystal Lite.”
Shawn Harris, CT Supervisor of Alamance Hospital in NC, testifies to his experience in the departmental change in working with Breeza 220 stating, “Since we started using Breeza, drinking compliance and image quality have been consistent and we’ve spent less time coaching patients.”
Created as a beverage for enterogrpahy exams, Breeza® flavored beverage for neutral abdominal / pelvic imaging (REF 221) is also sugar-free/gluten-free, has a light, refreshing, lemon-lime flavor, and a viscosity level that is 7x less than a barium-sulfate solution commonly used for this exam, that helps patients to drink the full amount.
Donna Pflugg's facility switched to Breeza 221 and told us,“The doctors like Breeza (221) for neutral abdominal/pelvic imaging. The patients drink within the time-frame and radiologists get the image they need. Everything’s where it's supposed to be in the bowel and they’re able to see what they need to see.”
 Physicians and clinicians from the Mayo Clinic in Rochester, MN evaluated a flavored beverage for neutral abdominal imaging (Breeza 221 for neutral imaging) to measure patient tolerance, efficacy, and willingness to repeat the drinking protocol. They published their findings in the May 2016 issue of the American Journal of Roentgenology.
Physicians and clinicians from the Mayo Clinic in Rochester, MN evaluated a flavored beverage for neutral abdominal imaging (Breeza 221 for neutral imaging) to measure patient tolerance, efficacy, and willingness to repeat the drinking protocol. They published their findings in the May 2016 issue of the American Journal of Roentgenology.
The study showed that Breeza® flavored beverage for abdominal / pelvic imaging has a similar side effect profile and results in equivalent small bowel distension compared with low Hounsfield-value barium suspension, "but subjects rated taste and their willingness to repeat the drinking protocol higher for the (Breeza) flavored beverage."
They went on to add that "Given the results of this study, we made a change in our clinical practice and used the flavored beverage (Breeza) as the preferred beverage for distending the bowel for CT and MR enterography performed in adults and children.”
If taste and texture are keeping you from obtaining an accurate image in abdominal CT imaging or in enterography, give the Breeza family of flavored beverages a try.
To learn more about setting up a trial evaluation at your facility for either Breeza 220 for use with oral iodinated contrast or Breeza 221 for neutral imaging in enterography, contact your Breeza Business Development Manager at 1-800-233-5539 or email info@beekley.com.
Acknowledgement: Thank you to Elizabeth Santoro, Senior Business Development Manager for contributing to this article
Related articles:

Jonathan McCullough
Product Manager
