Did you know that 67% of all female breast cancers occur in the upper outer quadrant of the breast? Did you also know that the largest percentage of quality failures cited by the MQSA are due to poor positioning? Of all those positioning failures, inadequate visualization of posterior tissue and/or the pectoralis major muscle account for nearly half.
Poor positioning is problematic for both patient and facility
When you take into consideration that mammographic images submitted for accreditation are selected by the facility, one has to assume the images chosen represent a "best foot forward" - the cream of the crop, so to speak. If those carefully chosen images are not passing quality standards, one has to wonder about the images not chosen for submission.
The FDA itself acknowledged the limitations of the clinical image review when it rolled out EQUIP (the Enhancing Quality Using the Inspection Program) - among which were the fact that clinical images were looked at every 3 years as part of re accreditation and that random image checks during on site MQSA inspections covered only a small percentage of facilities, despite the fact every certified breast imaging facility is inspected yearly. By putting the onus for quality on the radiologist and sending images collected at the yearly inspection to the accrediting body, the FDA hopes to reduce the number of additional mammography reviews resulting from poor clinical images.
In mammography, every millimeter counts. Imaging technology has improved to a point where microcalcifications as small as .2mm are detectable. If complete visualization of tissue in the area most breast cancers occur is missing, how many early signs of breast cancer are being missed due to poor positioning?
Positioning in mammography is especially challenging
Mammography is the hardest imaging modality to master - for both radiologist and technologist. Let's face it - positioning is hard, physical work. The mammography technologist is faced with the challenge of trying to get a perfect image every time under very imperfect circumstances and do it within a 15 minute time-frame.
In her 3 part series, "What Every Mammography Technologist Would Like Their Radiologist to Know About," Louise Miller, co-founder of Mammography Educators writes, "We often say that a good mammography technologist plays the role of health care professional, psychologist, educator, engineer, acrobat, and maybe, even a bit of a magician….all in about 20 minutes or less."
Patients, and their breasts, come in a variety of sizes and with varying levels of cooperation. Patients can have physical limitations that hinder the positioning process, breasts that may be too large to fit on one image or too small to stay under compression, their skin may be sweaty or too dry and prone to tearing, they may have implants, hate being compressed, or just plain scared or ornery.
Ms. Miller goes on to state that it takes months, even years, for mammography technologists to master all aspects of their responsibilities and their craft. To complicate matters, 10-15% of the patient population has limitations that will always result in sub-optimal imaging.
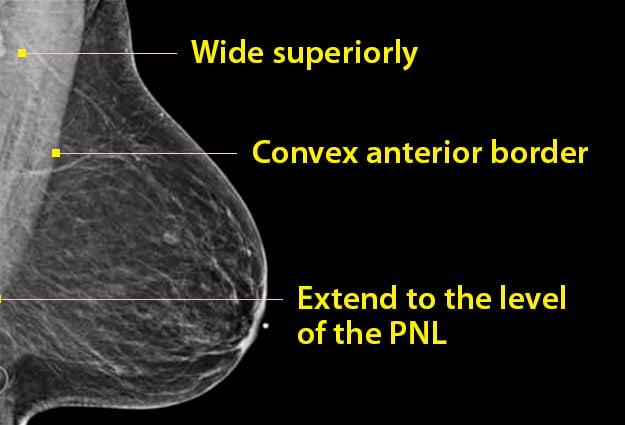
But, for the remaining 85%, the majority of images should meet ACR standards for proper positioning - including visualization of retro-glandular fat and the pectoralis major.
Optimal positioning for quality images a team effort
As mentioned earlier - the goal of the EQUIP initiative is to have the interpreting radiologist be responsible for the quality of the facility's mammographic images. This entails review of each technologist’s images and enacting corrective action if images fail. This can be in the form of case reviews, requirements for additional training in the specific criteria that constitutes acceptable images by the ACR and/or additional training on positioning, or investment in tools that can help boost tissue acquisition and help hold good positioning of the breast in place, once the technologist's hands have been removed.
Bella Blanket's® protective coverlets for mammography is one such tool. Aligning with EQUIP's proper positioning guidelines, 80% of Bella Blanket customers surveyed stated that they are capturing more breast tissue on their images compared to prior images where another product or no coverlet had been used.
In fact, a clinical study of 58 patient images demonstrated that in addition to helping technologists capture more breast tissue in 77% of patients, 48% of patients imaged showed improved visualization of the pectoralis major as outlined in the video below:
Bella Blankets protective coverlets for mammography - when every millimeter counts
Every millimeter counts™
The goal of every breast imaging facility is to not leave a cancer in the room.
Focusing on consistently meeting ACR image quality standards for mammography positioning will not only help facilities improve quality and decrease accreditation failures, it will also help detect more early stage cancers in the problematic upper outer quadrant.
To learn more about how Bella Blankets can help with your quality initiatives in mammography, contact your Account Manager at 1-800-233-5539 or email info@beekley.com.
For safety-related information on Bella Blankets, visit beekley.com
Related articles:

Mary Lang Pelton
Director of Marketing Communications
