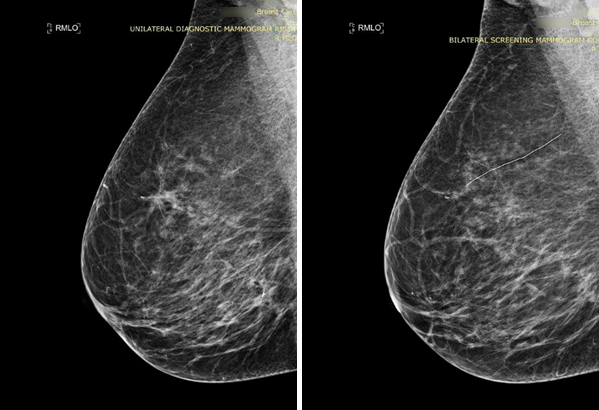
It is becoming more well-known that architectural distortion from old surgeries not seen in 2D can often be visualized in digital breast tomosynthesis.
When you see this newly appreciated architectural distortion you are faced with the need to explain it. How long has it been lurking there? Is it something new? Is it cancer?
The following case history is that of a 62 year old woman (Patient X*) with multiple excisional biopsies to both breasts over the years.
None ever proved to be cancer and as her physical scars faded, so did her memory of where her surgeries had been. She just remembered that she had several surgeries in both breasts at one time or the other.
The interpreting radiologist* is a breast imaging specialist who runs two breast centers serving a rural community in southern Kentucky. As is usual in small communities, the radiologist knows just about everyone. As a result, she is very passionate about delivering the best possible care to her patients. To her, mammograms are not just images on a screen, they're personal. It's hardly surprising she was an early adopter of digital breast tomosynthesis.
When she first began offering 3D mammograms to her patients, the radiologist stopped using skin markers for moles and scars. This decision was due to the equipment's algorithm which caused the dense wires and bbs (used to mark areas of interest like moles, masses, and scars) to blur on the computer-generated images that "fill in the gaps of missing information" between the sequences of actual imaged breast tissue. She found it distracting and feared it could obscure important tissue detail. Like many others, she felt this decision would have minimal, if any, impact on her images as the new technology allowed for much greater visualization of breast tissue than ever before in mammography.
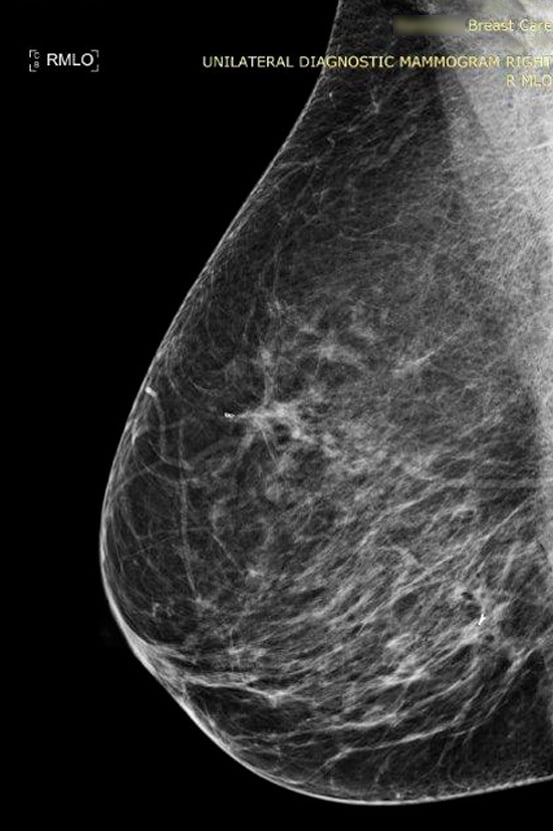
Troubling distortion- previous surgical site or something new?
When Patient X came in for her annual mammogram and first in 3D, the radiologist noted some architectural distortion, However, knowing the woman's history of previous benign excisional biopsies and seeing that it looks stable compared to previous years she attributed it to a prior surgery and makes her report.
The following year, Patient X returns for her annual mammogram. The radiologist sees the distortion again and thinks it looks just a tiny bit more prominent. It bothers her.
She looks at previous mammograms going back to 2009 (anything before that was film screen and unavailable to her). It still looks stable, but her instinct is screaming at her.
She asks Patient X to physically show her where her surgical scars are. The woman can't remember, and in the radiologist's own words, "She's is extremely white skinned; very, very pale" making it extremely hard to detect the scars on her breast.
After a very up close and personal examination of Patient X's breasts, the radiologist finally locates the physical scars.
The scars are located in the superior aspect of her breast. The distortion noted by the radiologist on the mammographic images is on the inferior.
Patient X undergoes another biopsy. This time, the pathology report shows it is cancer. A 5 mm slow-growing tubular cancer.
It was “A wakeup call.”
"It didn't change her outcome, but it does change the way you feel about how you do things. We really have to be marking this stuff. We have got to know where these scars are, because no matter how good tomo is, no matter how superior it is at detecting distortion, it cannot distinguish between a scar from surgery and a scar from cancer.You have to have a scar marker that tells you where the internal surgical scar should be so you don't let go of a cancer scar thinking it's a surgical scar. Scars need to be marked the 1st year after surgery and once you know where your scars are because you marked them the year before, you keep marking them. Year after year after year.”
According to the radiologist, breast radiology is an art. "There are always going to be slight differences anytime you compare two mammograms from the same patient. The breast radiologist's job is to determine if those differences are okay or if they could be early signs of cancer. We're constantly fine-tuning our library of normal and abnormal because the breast pattern is different in every woman. Normal breast tissue can look 100,000 different ways on a mammogram. If a breast radiologist can make that mistake, anybody can make that mistake."
Even if Patient X weren't the mother of a close friend, her case made the radiologist reconsider the impact skin markers have in mammography, even with digital breast tomosynthesis.
“Mammography, even 3D, does not catch all cancers. So being able to pinpoint where the pain is, where the lump is, and yes, where the old surgical scar is, is critical. I think it's really critical. We (radiologists) all have things like this happen to us and if we put our egos aside and share it with each other, we can help everyone do better. And that's really what it's all about - getting better at finding early cancers each day and saving lives. Sometimes it takes a while to figure out what you really need and what you really don't need. There are lots of reasons to use skin markers in mammography - every case that was either missed or delayed in their diagnosis because a marker wasn't used; or could have been missed if the not for the marker being there.”
Radiologists are struggling with the new realities of viewing images of patients with previous surgeries in 3D.
With older technology, the conventional wisdom was to mark biopsy sites every year for 5 years and then as the tissue healed and became less prominent, stop marking. Now, with tomosynthesis, older surgical sites are very evident, causing questions, concerns, and uncertainty.
Judgment calls need to be made and extra workups ordered. When breast specialists, who are much more adept at finding cancers than non-specialists, have concerns about false negatives or false positives associated with architectural distortion seen in 3D mammography, you can be sure it is an industry-wide concern.
Fortunately, scar markers exist that were developed specifically for optimal imaging in 3D mammography – sheer enough to see through and minimize distortion from the computer-generated images, yet just dense enough to communicate the important information about the excisional location of previous biopsies.
As more and more mammography facilities adopt digital breast tomosynthesis, marking post-surgical scars year to year should become a best practice.
*Names withheld for privacy purposes

Mary Lang Pelton
Director of Marketing Communications
