There has been much debate in the last few years regarding the use of positive oral contrast for patients with acute abdominal pain in the ED setting.
Typically, radiologists want oral contrast as it helps with the speed and accuracy of their diagnosis.
The ED physician wants to get the diagnosis right as well but they are also concerned with the need to disposition patients as soon as possible. The “treat them or street them” attitude is necessary as you never know when the next wave of emergent patients will walk through the doors or arrive by ambulance.
Time to scan a concern
There is much variance in the time different radiologists will wait from first sip of the oral contrast to the time they scan.
In the past, many hospitals adopted a longer prep time to ensure that the contrast had at least reached the cecum.
It is very difficult to get this first sip-to-scan time perfect as the patient’s size, disease state, and current bowel contents will all affect the transit time of the contrast. Times of 90 minutes to 2 hours and longer are not uncommon and this is considered unacceptable from the ED physician’s perspective. When IV contrast is used, as it often is, the patient will need a serum creatinine to clear the kidneys as well.
But oral contrast has its advantages
Since an acute abdomen is a potentially surgical patient, the use of a water-soluble contrast is preferred.
Gastrografin® and MD-Gastroview® are difficult for patients to tolerate due to the bitter taste. Due to the low osmolality of Omnipaque®, much of the fluid is absorbed by the time the contrast reaches the cecum resulting in an excessively bright image.1
Fortunately there is an easy solution to the time and taste problems that will satisfy the patient, the radiologist and the ED physicians.
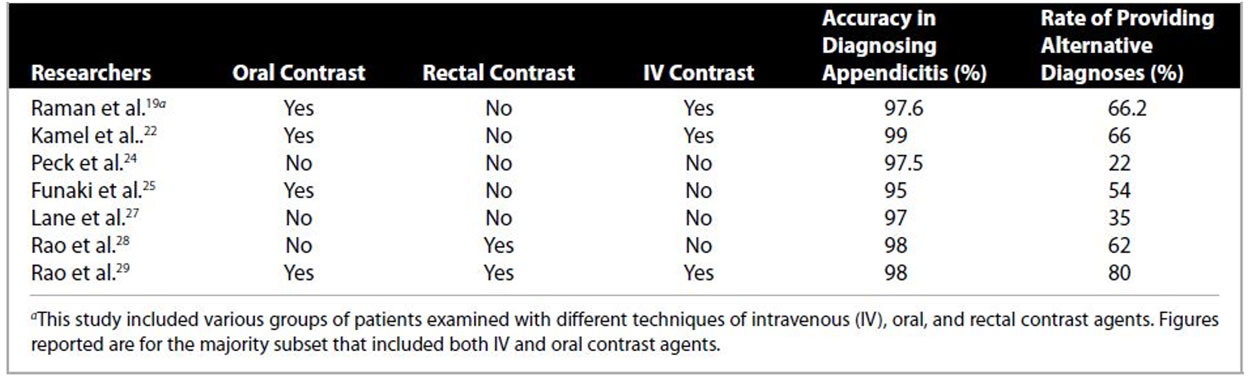
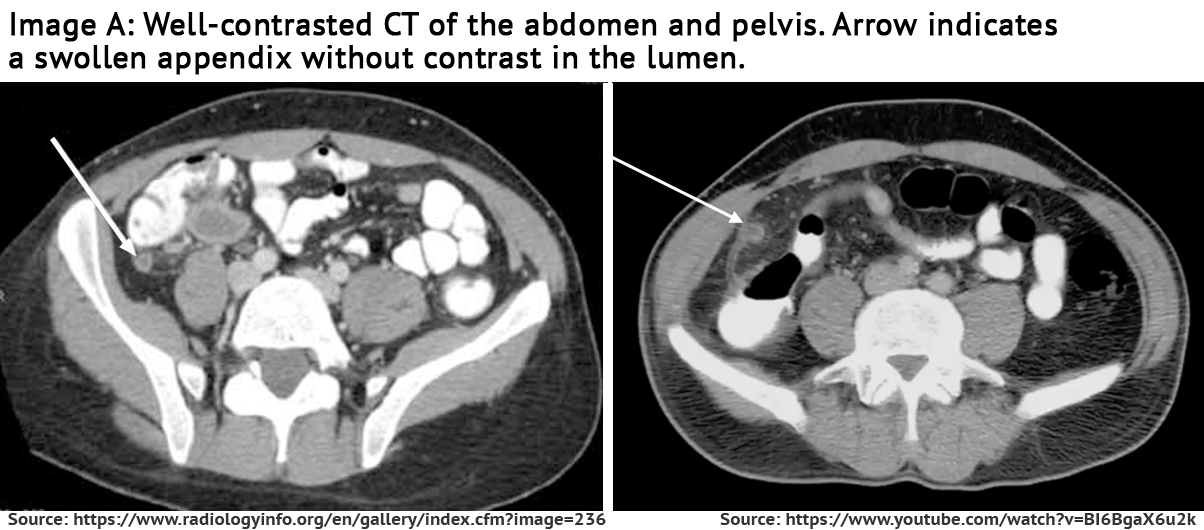
When a patient presents in the ED with an acute abdomen, CT is the modality of choice. CT has been proven to be effective in decreasing the negative appendectomy rates from 24% to 3%. (Image A)
What are the benefits of positive oral contrast when diagnosing the patient with the acute abdomen in the ED setting?
- A swollen appendix will not contain contrast.
- The radiologist can quickly differentiate the appendix from small bowel loops.
- Only 14% of acute abdomens are due to appendicitis
- Oral contrast will assist in the diagnosis of the other possibilities on the differential, such as Crohn’s disease, PID, pyelonephritis and small bowel obstruction.2 Evidence of this last point is seen in the table3 below:
Additional reasons for missed appendicitis on CT include misleading clinical history, paucity of intraabdominal fat, and incomplete opacification or absence of positive contrast4 as illustrated in the images below:
New beverage and suggested prep helps overcome challenges with "first sip to time to scan"
To solve the problems listed above while also providing the perfect prep for a routine CT of the abdomen and pelvis, many facilities have turned to Breeza® flavored beverage for use with oral iodinated contrast.
Breeza (Beekley Medical, REF#220) is specifically designed to block the bitter taste of Gastrografin and Gastroview giving you the perfect combination of a palatable drink that the patient will finish and the imaging characteristics the radiologist desires.
These facilities have also adopted the mixing and drinking protocol outlined by Dr. Peter Quagliano in the article "Contrast Mixing Protocol Improves GI Opacification on CT" published in Aunt Minnie on July 19, 20131.
article "Contrast Mixing Protocol Improves GI Opacification on CT" published in Aunt Minnie on July 19, 20131.
This article discusses a drinking protocol where a water soluble contrast is mixed with Breeza and consumed over a 60 minute period, with scanning starting between 70-75 minutes after first sip.
Considering this possible protocol, the evaluation of the patient with the acute abdomen could proceed in this way:
The ED physician evaluates the patient and writes orders to include some or all of the following:
- Labs to include CBC, electrolytes, amylase, lipase, BUN and creatinine.
- Urinalysis
- CT of the abdomen pelvis with oral and IV contrast
- IV fluids
- Pain medication
The attending RN proceeds to the med room and draws up the pain medication and mixes the oral contrast with Breeza.
Upon returning to the room, the patient is instructed how to drink the oral contrast. IV access is established and blood is drawn.
The patient can then give a urine and all samples are sent to the lab. The pain medication is given as soon as it is appropriate.
With a few exceptions, most in-hospital labs will take one hour to return routine results. Since the creatinine results are needed to clear the kidneys prior to the administration of the IV contrast, the patient cannot go to CT until they are returned.
If the above mixing and drinking protocol is followed, the patient will finish drinking the contrast just as the needed lab results are returning.
Mixing positive oral contrast with Breeza and following Dr. Quagliano's 60 minute drinking protocol increases the chances the patient will drink the entire amount of oral contrast in a time frame that will be acceptable to the ED physicians.
- Quagliano P. (2013 July 19) Contrast Mixing protocol improves GI opacification on CT. Aunt Minnie. Retrieved from: http://www.auntminnie.com/index.aspx?sec=sup&sub=cto&pag=dis&ItemID=104023
- [CTISUS]. Dr. Karen Horton, John’s Hopkins (2015, August 21). CT of the Acute Abdomen: GI Causes [Video File]. Retrieved from https://www.youtube.com/watch?v=gFhygT1WkXw
- [RadTechOnDuty]. Hiya II Lim, (2017, March 29) Protocols on Diagnosis of Appendicitis in CT Scan. Retrieved from http://www.radtechonduty.com/2017/03/protocols-diagnosis-appendicitis-ct-scan.html
- Levine et al, 2005 Why We miss the Diagnosis of Appendicitis on Abdominal CT: Evaluation of Imaging Features of Appendicitis incorrectly Diagnosed on CT. AJR; 184:855-859.
Related articles:

Richard Foster
Director of Training