
Approximately 1 million women in the United States undergo an image-guided core biopsy procedure as a result of suspected breast cancer each year.
The good news is that the results from the majority of these procedures turn out to be benign. The bad news - according to a study commissioned by the U.S. Department of Health and Human Services (HHS) is that an estimated 10,000 patients per year "experience a delay in diagnosis of their breast cancer due to a failure to resolve imaging pathology discordance after their biopsy."
The study goes on to list several contributing factors to this discordance, with technology and communication sitting at the top.
Advancements in technology a blessing and a curse
With today's advanced imaging equipment, radiologists routinely detect anomalies in the form of microcalcifications that can be very early stage breast cancer.
The benefit of being able to detect cancer in its earliest stages benefits the patient in terms of quality of life and long-term survival. The challenge for both radiology and pathology is that the smaller the finding - the greater the difficulty in sampling the lesion.
To illustrate this challenge, the authors of the article, "Stereotactic Breast Biopsy: Pitfalls and Pearls," laud the improvement in targeting accuracy of microcalcifications with the advent of vacuum-assisted core retrieval systems, but  also point out that despite radiographic images showing calcifications within core samples, there are cases where pathology fails to find calcifications within the specimen. "Calcifications within cores may be dissolved during processing or fall out of the tissue and be lost during cutting."
also point out that despite radiographic images showing calcifications within core samples, there are cases where pathology fails to find calcifications within the specimen. "Calcifications within cores may be dissolved during processing or fall out of the tissue and be lost during cutting."
Because these tiny lesions are so delicate and can cause discordant findings between radiology and pathology, both studies stress the importance of documenting the presence of calcifications in the core samples via a specimen radiograph at the time of the procedure and comparing the imaging results with the pathological findings to determine the next course of action for the patient.
Communication matters
The HHS commissioned study, "The Importance of Radiology and Pathology Communication in the Diagnosis and Staging of Cancer: Mammography as a Case Study," indicates that communication between these two partners in cancer detection suffers because they tend to work in siloed environments.
As an example of improved communication and workflow, the authors cite an integrated model implemented at UCLA during the time of the study and conclude that "Improvements in the collaborative workflow processes between radiologists and pathologists are critical in cancer diagnoses. Implementing a system or process that allows optimal communication exchange between radiology and pathology will provide immediate benefits for practitioners and patients."
5.5.2 Workflow of the integrated UCLA model
The report will be initialized by the interventional radiologist performing the biopsy. The radiologist will be responsible for linking the most appropriate diagnostic radiological study and radiological procedure with the pathology specimen.
This will ensure that the end-user will have access to the most relevant radiological studies when reviewing the pathology findings. The radiologist will flag and annotate pertinent images from the diagnostic radiology study for the Rad-Path report, and he or she will sign-out the radiology study which will also exist as a distinct radiology report in the hospital medical record.
To assist the radiologist and ensure adequate sampling, a cytotechnologist will be available in the radiology suite to perform adequacy checks on the specimen, partition the specimen as needed into appropriate specimen containers, and accession the specimen into the pathology laboratory information system. The pathology specimen accession number and the Rad-Path report number will be included within the body of the radiology procedure report.
Of course, not every facility can implement this type of work flow. The authors acknowledge that in many cases radiology and pathology may not even be housed in the same building. In fact, it's not unusual for facilities to send their specimens to off-site 3rd party pathology labs for processing.
Small, but simple ways any facility can reduce imaging/pathology discordance:
 But there are steps facilities can still take to minimize discordance of findings and improve communication between radiology and pathology.
But there are steps facilities can still take to minimize discordance of findings and improve communication between radiology and pathology.
- Minimize handling of cores to protect tissue integrity - as mentioned earlier, the microcalcifications within these core biopsy samples can easily become dislodged from the tissue sample at any point after collection. Minimizing the amount of handling as much as possible after collection can help improve the chances of the calcifications staying in place for pathology to process
- Clearly communicate findings of cores with calcifications - having the specimen radiographs showing that cores with microcalcifications were collected and the location of those cores in the specimen container will help determine concordance between imaging results and pathologic analysis and whether additional intervention is necessary
- Ensure patient information is clearly and accurately correlated with the core biopsy specimens - it shouldn't need to be said, but mistakes do happen on occasion in healthcare where information gets lost. Ensuring the radiographs and the specimen container are both labeled with patient information will help improve communication between radiology and pathology and reduce potential confusion and delays. The actual specimen container the cores are transported in should have the patient identification attached and not just the lid to that container.
CoreTainer® - the all-in-one system for stereotactic core biopsy specimens
Whether you use a basket core retrieval system or prefer manual core collection, there is a CoreTainer product that will help you improve communication between radiology and pathology.
Because you can image and transport in the same container, CoreTainer helps you minimize handling of delicate core specimens.
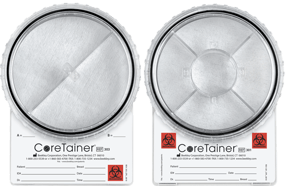 Microcalcifications are clearly visible on the image. Separate compartments allow radiology to place core samples as desired and help pathology correlate location of cores with calcifications to the specimen radiograph.
Microcalcifications are clearly visible on the image. Separate compartments allow radiology to place core samples as desired and help pathology correlate location of cores with calcifications to the specimen radiograph.
Each CoreTainer product is formalin-safe, has a watertight lid, and a section specifically for patient information so no need to transfer cores to another container after imaging in order to send the specimens to pathology.
To learn more about CoreTainer stereotactic core biopsy image and transport systems (A/B divider for basket collection; clock-face divider for manual core collection) or to request samples for evaluation, contact your Beekley Medical Account Manager at 1-800-233-5539 or email info@beekley.com.
Visit www.beekley.com for product safety information
Related articles:

Mary Lang
Director of Marketing Communications


