Transthoracic needle biopsy (TTNB) is integral in the diagnosis and treatment of lung cancer.
 TTNB is usually performed under CT image guidance by a radiologist as it is less invasive than most surgical alternatives.
TTNB is usually performed under CT image guidance by a radiologist as it is less invasive than most surgical alternatives.
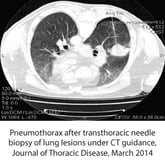
While TTNB plays a crucial role in diagnosis of lung cancer, it is not without risk. Morbidity is very low (occurring less than 1% of the time), but other risks include chest tube placement, hemoptysis, and pneumothorax – the collapse of the lung. Pneumothorax is the most common and occurs in 20% of needle biopsies.
Factors That Increase Risk of Pneumothorax
There are many complications that can increase the risk of pneumothorax.
The patient’s health should be considered when planning for the procedure. Patients who have (or have a history of) emphysema, chronic obstructive pulmonary disease (COPD), prior treatment for lung cancer, or a history of past surgeries tend to be at a higher risk than those without.
Furthermore, the size of the lesion, a long needle path, and repeated pleural punctures – or taps – are also a factor in determining the risk of pneumothorax occurring in a patient. If pneumothorax does occur, chest tube placement is likely and the patient may be held overnight.
Choosing the Right Tool to Localize Needle Entry Point for First–Stick Accuracy in TTNB
While there are several methods employed in interventional CT for localizing the needle entry site, each one has its pros and cons and varying degrees of consistent, repeatable, accuracy.
►Makeshift or home-made grids:
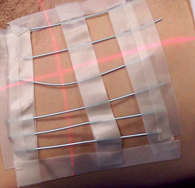 Usually made of tape and wire, or tape and cannulas, within the CT department, these home-made grids are obviously inexpensive and the materials to make them are most likely always on hand.
Usually made of tape and wire, or tape and cannulas, within the CT department, these home-made grids are obviously inexpensive and the materials to make them are most likely always on hand.
The downside to home-made grids is that they are time consuming to make, their construction and precision is dependent on the skill of the technologists making them, and they are often reused – increasing the risk of infection to a patient who may already be sick.
►A single pellet or BB-style localization marker:
Most pellet or BB-style markers usually professionally made with the marker sitting atop an adhesive backing. Professionally made localization markers are intended for single-use only with infection control in mind. Some of these pellet-style markers are created specifically for diagnostic CT to reduce scatter artifact seen when denser or metallic markers are used.
In this method of using a single BB to determine the needle entry site, the patient is taught a breathing technique where the image is captured while the patient holds their breath in full expiration.
Due to the difficulty pulmonary patients have replicating this breathing technique it is often difficult capturing the BB on the desired slice. If the patient “breathes off the mark,” additional attempts will be made leading to unnecessary radiation dose and increased procedure time.
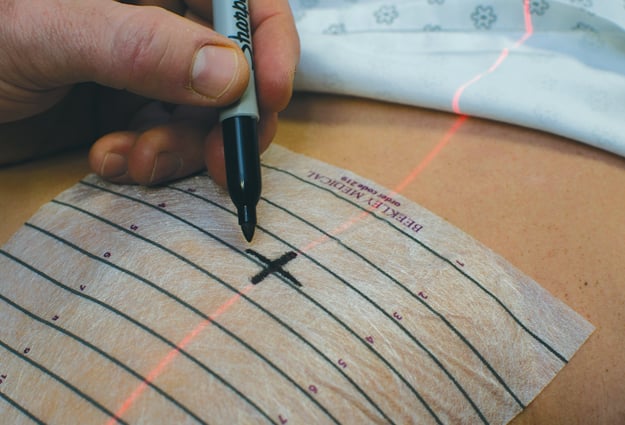
►Professional, self-adhesive biopsy grids
This last category represents the most precise and accurate way to identify needle-entry sites.
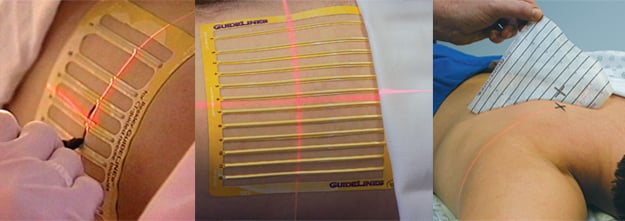
These professional grids, intended specifically for CT-guided biopsy procedures, are precision-engineered to have uniform spacing between the lines and clear indicators for measuring back on the CT Image. They are designed to image with minimal scatter, making it quick and easy for the radiologist to identify his needle entry point and pathway.
It is important, however, to keep in mind that not all professional biopsy grids offer the same benefits to the imaging team and the patient.
Some CT-Biopsy grids do not have a fully adhesive backing and can buckle, or lift, off the patient’s skin during imaging -reducing accuracy and making it difficult to correlate the localization mark to what is seen on the image.
Fully adhesive CT-biopsy grids like Beekley Medical’s GuideLines® and Mark-Through GuideLines® contour to the patient’s anatomy without buckling, helping to ensure the mark on the skin corresponds to the appropriate grid line in the CT image.
Precision in Planning Helps Reduce Risk
This precise localization of the needle entry site for CT-guided biopsies of the lung not only increases the accuracy of the procedure, but also decreases the likelihood of multiple passes or additional scans for the patient.
If you are looking to achieve first-stick accuracy in your CT-guided transthoracic needle biopsy procedures, give the GuideLines® family of CT-biopsy grids a try.
Contact your Beekley Medical business development manager for Advanced Imaging at 1-800-233-5539 or info@beekley.com to inquire about a trial evaluation to compare to your current method of identifying needle entry sites.

Jonathan McCullough
Product Manager


