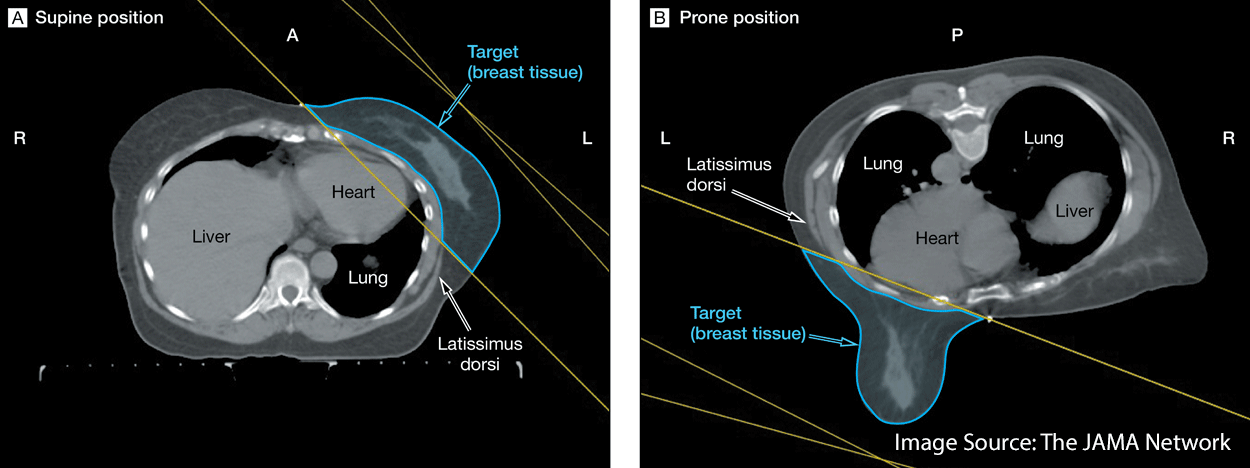
The standard of care for post-lumpectomy breast cancer patients has been the delivery of whole breast radiation in the supine position. However, there is significant evidence that the heart and lungs are organs at risk (OAR) for radiogenic problems in long term survivors when treated in the supine position.1,2
Additional challenges posed by the supine set-up include the tendency for a large breast to dislocate laterally (making reproducibility of the simulation position difficult) and the potential for a bolus effect at the inframammary fold due to skin on skin contact.3 Patients with large pendulous breasts and an increased body mass index were also at risk for radiation related toxicity when set up in the supine position.4
Concavity vs. Gravity
These challenges of the supine set-up arise due to the concave nature of the whole-breast clinical target volume.
In a left-sided cancer this volume wraps anteriorly around the heart and lung towards the right breast medially.
When treating the right breast, the right lung is at risk. Left breast cancers put the left lung at risk as well as the heart, specifically the left anterior descending coronary artery (LAD).
Because the heart and lungs often fall within the treatment field in the supine set up, the prone position has been explored as an alternative.
Prone positioning takes advantage of gravity to displace the breast to be treated away from the chest wall into an opening in the breast board or table. The contralateral breast is moved laterally on top of the table. 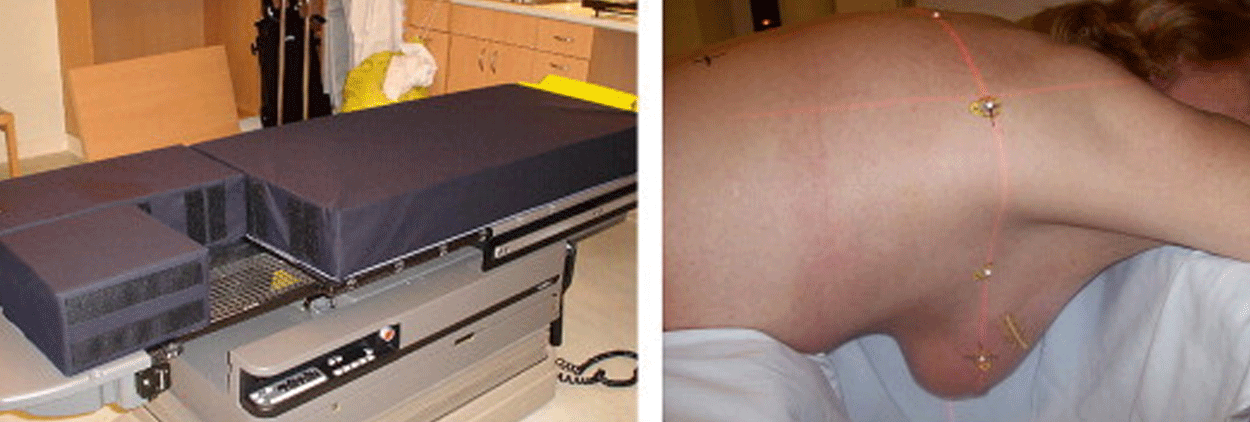
Less radiation risk to organs
A 2013 study by Mulliez et al. found that, “Prone IMRT was superior to any supine treatment for right-sided breast cancer patients and left-sided breast cancer patients with larger breasts by obtaining better conformity indices, target dose distribution and sparing of the organs at risk.” 5
With regard to cardiac toxicity, a study published in Radiotherapy and Oncology in 2010 looked at supine versus prone set-ups and the dose to the ipsilateral lung, heart, and LAD.
In this study, large breasted patients with left breast cancers were more likely to experience cardiac benefits from prone positioning, while patients with smaller breasts were not. If the patient had a right sided cancer they could benefit from prone positioning regardless of their breast size.6
Lymberis et. al. performed a CT simulation in both the prone and supine position on 100 patients to determine the best possible set up to avoid dose to the OAR. They found that regardless of the breast affected, prone positioning was superior to supine with regard to lung dose.
Additionally, 87% of left breast cancer patients had a lower in-field heart volume exposed.7
Of course, prone set-up for breast patients has its drawbacks as well. Elderly patients have difficulty tolerating the prone position and it requires longer set-up times.
Regardless of set-up position, reproducibility is key
In addition to determining the best position to simulate and treat the patient it is important to ensure reproducibility.
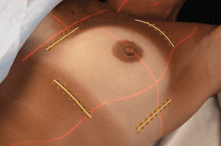 Beekley Medical's CT-SPOT® pellet, crosshair, and line skin markers image consistently minimize artifact during treatment planning. PointGuards® temporary mark protectors provide a watertight seal and stay securely in place for up to 4 weeks, reducing the likelihood of having to resimulate the patient during treatment.
Beekley Medical's CT-SPOT® pellet, crosshair, and line skin markers image consistently minimize artifact during treatment planning. PointGuards® temporary mark protectors provide a watertight seal and stay securely in place for up to 4 weeks, reducing the likelihood of having to resimulate the patient during treatment.
References:
- Moody AM, Mayles WP, Bliss JM, et al: The influence of breast size on late radiation effects and association with radiotherapy dose inhomogeneity. Radiother Oncol 1994, 33(2):106–112.
- Mulliez et al.: Whole breast radiotherapy in prone and supine position: is there a place for multi-beam IMRT?. Radiation Oncology 2013 8:151.
- Levi F. et al.: Cancer risk after radiotherapy for breast cancer. Br J Cancer 2006; 95:390-392.
- Kirby, Anna M. et al. Prone versus supine positioning for whole and partial-breast radiotherapy: A comparison of non-target tissue dosimetry. Radiotherapy and Oncology 2010, Volume 96 , Issue 2 , 178 - 184
- Early Breast Cancer Trialists’ Collaborative Group (EBCTCG). Effects of radiotherapy and of differences in the extent of surgery for early breast cancer on local recurrence and 15-year survival: An overview of the randomised trials. Lancet 2005;366:2087–2106.
- Krengli et al.: Prone versus supine position for adjuvant breast radiotherapy: a prospective study in patients with pendulous breasts. Radiation Oncology 2013 8:232
- Lymberis, Stella C. et al.: Prospective Assessment of Optimal Individual Position (Prone Versus Supine) for Breast Radiotherapy: Volumetric and Dosimetric Correlations in 100 Patients. International Journal of Radiation Oncology 2012
Related articles:

Richard Foster
Director of Training


