
It is no secret that the healthcare sector has had an increased focus on the patient experience and their satisfaction. Hospitals, especially, are always considering ways to improve the patient experience as reimbursements are based on patient HCAHPS survey scores.
Hospitals have become creative over the years with self-playing Steinway pianos, restaurant-like cafeterias, beautiful artwork, waterfalls, and the list goes on. A lot of money, resources, and studies go into implementing these features to (hopefully) help the patient and their family feel more relaxed and have a good experience when in the hospital.
How frontline staff can impact the patient experience:
It only takes one staff member to potentially impact that positive experience.
A staff member may be having a bad day, is coping with stress, or just immune to their setting and their interaction may be perceived by the patient as uncaring. Since the patient remembers how they felt during their stay, that staff interaction will most likely be included on their patient experience survey, impacting scores and reimbursement.
Hospitals realize that in order to have happy patients, you must have a happy, engaged staff.
The study, “Nursing: A Key to Patient Satisfaction” examined the relationship between with nursing and patient satisfaction HCAHPS scores in over 430 hospitals.
It proved that the nurses’ work environment was significantly related to the HCAHPS patient satisfaction surveys. It also determined that improving the nurses’ work environment could increase survey scores. Most notable was the global rating of the percent of patients who would definitely recommend the hospital.
Not only are patient satisfaction scores influenced by staff, so is the patient’s health. Another study, “Healthcare Staff Wellbeing, Burnout, and Patient Safety: A Systematic Review” concluded that staff who experienced poor well-being or burnout had a greater effect of poor patient outcomes.
Hospital frontline staff – how happy are they?
 Hospital frontline staff may endure a full day of caring for their patients that may be sick or dying and manage the patient’s family.
Hospital frontline staff may endure a full day of caring for their patients that may be sick or dying and manage the patient’s family.
They then go home to their “2nd job” of managing their family (crying babies, snippety teenagers, caregiver for an elderly parent) and managing the household (paying the bills, cleaning the house, cooking dinner).
While many of us also have that 2nd job after our career-day ends, hospital staff have stresses that outnumber many other professions. 92% of nurses report moderate-to-very high stress levels.
Depression is another concern among healthcare professionals. According to the American Foundation of Suicide Prevention, the suicide rate is 1.4 times higher in male physicians compared to the general male population. The suicide rate for female physicians is 2.27 times higher than the general female population.
How do you help frontline staff cope and keep them happy?
Keeping the staff happy starts with the C-Suite recognizing that the well-being of the staff is dependent on having programs in place to positively support their overall mental and physical health without judgment.
Dr. David Feinberg, CEO of Geisinger Health at the time of this writing, wanted staff members to feel they had purpose and were empowered at the UCLA location.
He changed the mission statement to read “Healing human kind one patient at a time by alleviating suffering, promoting health, and delivering acts of kindness.”
Programs in Place to Support Hospital Staff’s Well-Being:
- Aurora Healthcare of Milwaukee has the Tender Loving Care program to reduce stress, fatigue, and depression. They offer massages, aromatherapy, reiki, healing touch and nutrition support.
- Helen DeVos Children’s Hospital holds an emotional debriefing session for staff 24-48 hours after a traumatic event happens with a patient.
- St. Joseph Hospital of Orange, California has a Code Compassion program holding regular meetings for staff to talk openly about their experiences with patients.
- The Cancer Centers of America (CTCA) at Midwestern Regional Medical Center have “renewal” rooms dedicated to self-reflection and healing.
- Code Lavender at Cleveland Clinic is used as a crisis intervention program that both patients, family members, volunteers, or staff can take advantage of. A Code Lavender can be called at any time when a stressful event occurs and within 30 minutes the Code Lavender team responds. Code Lavender uses evidence-based relaxation and restoration interventions. The holistic team steps in and offers reiki, meditation, and massage, just to name a few.
There are many options to incorporate into the hospital environment to support the well-being of the staff.
Having a go-to place to decompress and relax seems to be a common theme and gives the staff member an opportunity to “get away” to re-energize.
Another form of relaxation gaining popularity is the use of aromatherapy within the clinical setting for both patients and staff; helping to cope with anxiousness.
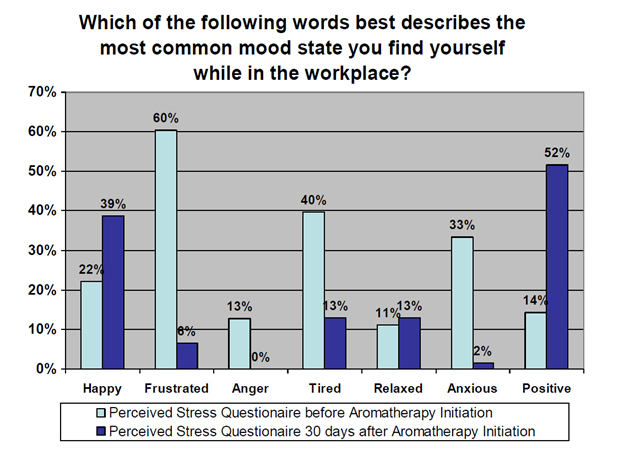
The Wellness Committee at Vanderbilt University Medical Center conducted a study on stress and mood among staff in the ED. Staff were monitored before and after using aromatherapy and found that staff anxiousness reduced 94% in 30 days with the use of inhalation aromatherapy.
Here were the results:
Aromatherapy “on the go” can help reduce anxiousness as the staff encounter stress throughout their day.
Elequil aromatabs is an easy-to-use option that adheres to scrubs, clothing, or to the back of an identity badge to be discreet. It is hands-free, stays within the zone of the person wearing it, offers MIN/MAX scent exposure, does not contain metal/foil, and travels with the person during their shift. It is a solution to support well-being during stressful events.
The first time I learned about the concept of putting staff first leads to better patient care and experience was at the Next Generation Patient Experience conference five years ago. I highly recommend this show for anyone looking to positively impact their staff and patients.
Visit Elequil.com or email info@beekley.com to learn more and request samples to evaluate how Elequil can help support your staff stress-reduction strategies.
Related articles:

Melissa Vibberts
Director of Brand Management


